November 16, 2022
Digital therapeutics 2023: Swing and trial partner Curavit kick off fibromyalgia study
Media Coverage | EndPoints News
January 12, 2023
After the boom-and-bust cycling in digital therapeutics over the past few years, digital health providers are looking for 2023 to be a stabilizing year. Two of those companies are digital therapeutics developer Swing Therapeutics and all-virtual CRO Curavit Clinical Research.
The pair are currently enrolling a trial for Swing’s Stanza, a prescription smartphone DTx for fibromyalgia. The cognitive behavioral therapy treatment, which received a breakthrough device designation from the FDA in 2021, became available for patients in September, alongside the formal clinical trial which will finish enrollment soon with the study set to complete in the third quarter.
“This is the first of multiple digital therapeutics for us. We’re targeting other chronic pain conditions that can be related to fibromyalgia – central sensitization syndromes is what they’re called,” Swing Therapeutics CEO Mike Rosenbluth said in an interview.
Swing is taking a different approach in digital therapeutics to help advance adoption. It’s developed an affiliated physician-owned telemedicine clinic, Swing Care, to “bridge the gap between patient awareness and access to Stanza,” Rosenbluth said.
For Swing, instead of creating a big salesforce to go out and educate physicians, patients can access Stanza, if appropriate, directly through the dedicated clinic, he said.
Another innovation is its use of virtual clinical trials through Curavit. Swing is Curavit’s tenth digital therapeutics client in fewer than six months, said Joel Morse, Curavit co-founder and CEO, with DTx companies making up about half of its client base.
Curavit has engineered a way for patients to never have to go to physical sites. While the Swing fibromyalgia study participants do have an option to participate in-person and digitally, the Curavit enrollees join the trial and engage with study coordinators and investigators entirely through telehealth.
Rosenbluth said Swing did have questions about running trials remotely and an initial concern that engagement might not be as high with patients never having to show up somewhere. That hasn’t been the case, though.
“Patients participating from Curavit’s site are just as engaged or even more so than the average patient in our studies in terms of compliance, patient reported outcomes and with the digital therapeutic itself,” he said.
Virtual Site Brings Speed, Diversity, And Engagement To Digital Therapeutic Trial
Media Coverage | Clinical Research News
January 11, 2023
Digital therapeutics (DTx) are a natural fit with the decentralized clinical trial (DCT) model and the COVID-19 pandemic has been a major driver of demand for both. The hybrid-designed PROSPER-FM trial is a good case in point. The devices being studied are a digital Acceptance and Commitment Therapy (ACT) program and digital symptom tracker for adults with fibromyalgia, a surprisingly common and chronic affliction, and the single virtual site, run by Curavit, has been enrolling 10 times more patients than all other bricks-and-mortar sites starting at the same time.
That’s what’s being reported in a status update on the trial by Mike Rosenbluth, Ph.D., CEO of sponsor Swing Therapeutics and Joel Morse, cofounder CEO of Curavit, the world’s first all-virtual contract research organization (CRO). They agree that inclusion of the virtual site is proving to be a great way to broaden access to the study and enhance diversity while improving participant engagement overall.
The hybrid approach was a “smart strategy” by Swing, allowing the startup to balance the risk of betting on the wrong distribution channel before the evidence was in, says Morse. The virtual approach is still new and, understandably, the industry wants to see the data demonstrating its efficacy.
It’s looking good so far, says Rosenbluth, and not just in terms of enrollment. Participants are also staying in the trial and adhering to the protocol. The risk going in was that patients enrolled remotely could be less engaged and thus less likely to know, and do, what they’re supposed to. That the opposite has happened has been “really interesting.”
The enrollees recruited remotely include notoriously hard-to-reach populations, notably Native Americans located nowhere near a physical site, Morse says. Part of the trick is doing the upfront work of making the entire process virtual so individuals can truly participate in the trial from the comfort of their home.
Curavit, like Swing Therapeutics, is a young company. It was founded in early 2020—right before COVID-19 was declared a pandemic—to focus on DCTs, says Morse. Previously, he founded a company called C3i (sold to Merck in 2014 and subsequently purchased by HCL Technologies Limited) that grew into a $100 million global firm that split its time on global clinical trial execution and pharmaceutical commercial services.
That gave Morse 15 years of experience building out the service offering of Quintiles (now IQVIA), then C3i’s biggest client, as well as all of Medidata’s tier 1 and some of their tier 2 global core services. During this period, he also had plenty of practice running global clinical trials for sponsor companies big and small.
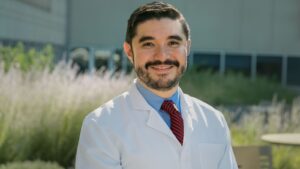
After getting his Ph.D. in biomedical engineering, Rosenbluth blazed his career path in early-stage venture investing with a focus on startup medical device and biopharma companies. Swing’s acting chief medical officer was also responsible for the last drug (milnacipran) approved for fibromyalgia in 2009, he notes.
Stanza, the prescription digital therapy app designed to deliver behavioral therapy to people with fibromyalgia, is the lead product of Swing Therapeutics, founded in 2019. But the company is also exploring other therapeutic areas, including several autoimmune diseases, where digital therapeutics can make a difference.
Scaling Treatment
The prescription DTx under investigation in the PROSPER-FM trial provides an innovative form of behavioral and cognitive therapy that is a first-line treatment for fibromyalgia, a widespread pain condition affecting 10 million people in the U.S. In addition to chronic pain, afflicted individuals can suffer from a host of comorbidities such as disturbed sleep, difficulty concentrating, and mental health impacts that include depression and anxiety, explains Rosenbluth.
Three drugs for treating fibromyalgia have been approved by the U.S. Food and Drug Administration (FDA): pregabalin (Lyrica, Pfizer), duloxetine HCL (Cymbalta, Eli Lilly), and milnacipran (Savella, Forest Labs/Cypress Bioscience). Prescription drug therapies have widely varying degrees of effectiveness but, even if they work, many patients opt to stop taking these drugs within a year because of intolerable side effects, Rosenbluth says.
In a public meeting with the FDA, patients reported that non-pharmacological approaches proved more reliably effective. Cognitive behavioral therapy with ACT—the aim of which is to help people accept their feelings as they are and commit to taking useful action in line with their personal values—has also been scientifically demonstrated to have positive effects on pain-related functioning, mental health-related quality of life, self-efficacy, depression, and anxiety (European Journal of Pain, DOI: 10.1002/j.1532-2149.2012.00224.x)
Scaling this “very specialized treatment” to accommodate the large population of patients with the disease has been the main challenge, says Rosenbluth. Swing’s answer was to develop a smartphone-based application to deliver the treatment digitally. And it received a Breakthrough Device designation from the FDA in hopes of more quickly bringing the product to market by creating an open, ongoing dialogue with the agency to ensure the evidence being built with the PROSPER-FM trial aligns with regulatory expectations of a submission package.
Prescription DTx are regulated as medical devices under the FDA’s Software as a Medical Device program, Rosenbluth says. Nine such devices have been approved to date.
Protocol Reengineering
The 12-week PROSPER-FM study started in February 2022 with 25 physical sites and a goal of enrolling up to 300 participants, says Rosenbluth. Participation requires six patient visits, and the primary endpoint is patient global impression of change per electronic patient-reported outcomes.
The study is expected to finish enrollment in the first quarter of 2023, Rosenbluth continues. Curavit was added to the mix in August with the expectation that its digital outreach approach would expand access to a broader patient population than would typically participate in clinical research by virtue of geography.
Adding a virtual site required making a few adjustments to the study workflow, says Morse. This most notably included reengineering of the one-step screening process requiring a urine drug screen and confirmation by the principal investigator (rheumatologist) that a would-be participant has fibromyalgia. For remote participants, the three-step procedure is for clinical research coordinators to conduct a 90-minute telehealth visit to screen individuals (eliminating half of the pool of prospects), who then go to a nearby drug center with a QR code to get a urine drug screen and subsequently have a televisit with the rheumatologist (again cutting the patient pool by 50%).
The changes were necessary for the virtual part of the trial to work to ensure appropriate individuals were enrolled as well as remove unnecessary burdens on patients, Morse says. Other than better reaching several underserved populations, he adds, people enrolled remotely looked very similar to those enrolled by the bricks-and-mortar sites. But, overall, they interacted more with the virtual site than their counterparts enrolled at a traditional research site.
While the virtual site has certainly augmented enrollment, the bricks-and-mortar locations are likewise indispensable when it comes to ensuring diversity, Rosenbluth says. “We are also relying on sites that are very experienced in conducting fibromyalgia studies and can help all the sites as they learn from each other, and Curavit has been able to take advantage of some of those learnings, too.”
From the FDA’s standpoint, a chief concern with remotely enrolling participants is identify verification, which represented a protocol amendment, says Rosenbluth. But, broadly speaking, the agency views DCTs favorably due to its interest in equitably expanding trial access.
The DTx industry, through regulatory guidelines and with the support of the Digital Therapeutics Alliance, is “working hard” to ensure its collective voice is heard with the FDA, Morse adds. “Frankly, regulators have been very open to hearing that voice and partnering… for the good of everyone.”
It’s a group that would be difficult to ignore. The global DTx market, valued at $42 billion in 2021, is projected to reach $56 billion over the next five years with an estimated compound annual growth rate of 26.1%.
In the U.S., the DTx market is expected to hit $11.2 billion by 2030. One of the drivers has been the FDA’s pandemic-related fast-tracking of commercial availability for prescription DTx products for treating patients with psychiatric conditions under the agency’s Enforcement Policy for Digital Health Devices during the COVID-19 Public Health Emergency, says Rosenbluth.
Gaining Traction
Digital therapeutics have many advantages—notably, no issues with shipping, storage, chain of control, cold storage, or biohazards, plus endpoints can often be captured within the DTx application itself. Yet DTx products face challenges including lack of physician awareness and the inability of doctors to easily prescribe them to patients, says Rosenbluth.
The questions looming large are how to convince physicians to prescribe a technology they’re unaccustomed to, and how to get payers on board so the device is a reimbursable expense. At Swing, the answer was to establish Swing Care, an independent online virtual medical practice devoted to the holistic treatment of fibromyalgia patients that is now operating in Texas and will expand to other states over the next year.
Clinics can prescribe traditional medications as well as digital therapeutics, Rosenbluth points out. Stanza is currently commercially available, ahead of marketing clearance, under the FDA’s Enforcement Policy for Digital Health Devices during the COVID-19 Public Health Emergency.
The parallel in the PROSPER-FM trial, he says, is the use of the 25 sites to distribute digital therapeutics to patients. In lieu of relying on a traditional CRO, Swing Therapeutics is working directly with those sites to remedy any issues they encounter and better understand the patient experience.
“Patient compliance is really important,” adds Rosenbluth, which is about keeping individuals engaged and supporting them through the study process (e.g., text message reminders). Swing has also learned from Curavit the value of digital recruitment campaigns, such as targeted ads on Facebook, Reddit, and Twitter, and plans to implement those approaches on the commercial side of the business.
Industry Predictions For 2023
Media Coverage | PharmExec.com
December 28, 2022
Top industry experts weigh in on what the new year holds for the pharma industry.
PREDICTION #1: In 2023, the chasm will widen between those companies investing in analytics-based, digital-first commercial models and those still sitting on the fence and taking a measured approach

Alan Kalton
Life sciences companies are notoriously cautious. However, COVID-19 put many companies in the uncomfortable position of forcing new ways of working, engaging with customers, and new technologies. For many companies, the changes are sticking, ushering in the digital-first era.
We have started seeing the impact of the adoption of new technologies, such as platform intelligence solutions, ‘on the ground.’ In fact, 89% of companies surveyed by DHC Group reported that they are successfully executing an AI-driven omnichannel strategy across sales and marketing and scaling up.1
Gone are the days when digital and analytics technologies were merely a shiny new toy to test-run in isolated markets. Today, many companies understand the impact of AI and recognize that it needs to be powering engagement across all markets. As the global director of field force AI enablement at Novartis noted recently during our Omnichannel AI Masterclass, “in three to five years, I hope that our industry has moved to where AI isn’t a buzzword, but rather, it’s baked into the mainstream of our go-to-market strategies because it’s so essential.”
The organizations delaying investment in scaling intelligence platforms across the organization will see a widening gap between them and their competitors in terms of influence, customer engagement and ultimately, financial success.
PREDICTION #2: Companies will connect data science models to day-to-day operational activities to execute on strategic business goals across the entire organization

Next year, we will see the start of the next chapter in AI for life sciences commercial organizations.
Traditionally, AI has lived in one of two places–either with headquarters teams, analyzing massive amounts of data to generate ‘smart’ conclusions, or within discrete applications, helping to tune the application’s impact (i.e. marketing automation systems). At headquarters, AI is used to strategically assess business opportunities on a broad scope whereas the tactical AI embedded into individual applications is very specific and application limited.
Both are valuable, but what’s missing is the connective tissue between HQ’s broad-scope AI to the various operational systems required to execute HQ’s strategic business goals. Such connective capability would reach into the multiple operational systems required for execution and guide the appropriate actions. As a result, operating teams could agilely deploy data science models to guide a wide range of day-to-day activities.
Ultimately, companies will be both more effective (more good decisions) and more efficient (less bad decisions that waste resources), cycling through the “try it, fix it” rhythm much faster to continuously improve AI’s outputs across the entire organization.
PREDICTION #3: AI-driven identification of digital opinion leaders (DOLs) will accelerate evidence dissemination

Medical Affairs teams are racing to provide a personalized “Netflix-like” engagement for ever-expanding targets, predicting needs and preferences and then delivering unbiased scientific information in the most useful formats and channels. Field medical affairs or medical science liaisons (MSLs), work to engage with physician key opinion leaders (KOLs), but also have a new target: digital opinion leaders.
DOLs, in essence, are KOLs active on digital platforms. DOLs may be practicing or non-practicing HCPs but have major influence over consumer behavior and informing other physicians. Some rise to near-celebrity status, such as Dr. Mikhail Varshavski–better known as Dr. Mike–who has a combined social media following of over 21 million people. He has been featured in Time, Men’s Health, Business Insider, and People Magazine, to name a few. Also, Dr. Don Dizon is a professor at Brown University and director of medical oncology at Rhode Island Hospital who shares cancer research via video primarily on TikTok. He has 38,000 followers.
In addition to doctors, nearly 90% of all adults in the U.S. search for health information on Facebook, Twitter, YouTube, and other social media sites. From doctors to patients, MSLs can multiply their influence by engaging with the right DOLs. AI and natural language processing technologies can help by mining available information–based on specialty, therapeutic area expertise, followers, outreach network, and posts–to help identify the right influencers to engage and cultivate a relationship.
Next year, as the role of the MSL continues to expand and evolve, MSLs will demand new smart technologies to help them engage with the growing fleet of digital influencers. And when these relationships are formed, MSLs will increase education and information dissemination faster and farther than they have ever done before.
PREDICTION #4: Decentralized clinical trial market will continue to grow, even in economic downturn

Industry leaders are debating whether or not decentralized clinical trials (DCTs) will become the norm rather than the exception across therapeutic areas–but, it’s neither. In 2023, the question will no longer be an “either/or” scenario. There will always be some trials and some elements of a trial that should not be decentralized. In 2023, however, the first question all sponsors will consider at the start of protocol design will be “what aspects of the trial can be decentralized.”
For some trials, the answer may be “all of them,” and for other trials, such as highly complex oncology trials, the answer may be “very few of them” as each trial has unique needs. However, with the rapid maturation of digital technologies and increasing comfort level with digital tools by patients and doctors, sponsors will adopt a digital-first mindset for every trial.
Digital technologies will be considered from the start rather than force-fitting them into a trial mid-way, which will ensure a more successful trial design overall. The financial and time savings of the DCT model, coupled with the remarkable patient benefits of greater access, increased convenience, and optionality, are too compelling for sponsors not to lead with it for each trial they invest in.
PREDICTION #5: Digital therapeutics companies will focus on the difficult last mile to commercialization

Historically, digital therapeutics (DTx) companies have directed about 95% of their effort into gaining FDA approval and 5% into market access strategy. In 2023, this will shift to a 60%/40% split, with DTX companies having an earlier focus on the commercialization process, while simultaneously working toward earning FDA approval.
This ‘last mile’ is completely unchartered territory for DTx companies.They face new obstacles bringing their therapeutics to market. For example, physicians’ lack of awareness of the DTx and their inability to easily prescribe them. There are still many unknowns around getting DTx products on the formulary and how to prescribe them to patients–doctors can’t just write a prescription and send patients off to the local drugstore when prescribing the use of an app.
And, whereas traditional drug companies may spend up to $300 million to launch a product, most DTx startups don’t have the budget to spend on commercialization strategies such as building a field team, equipping marketing teams with supporting analytics technology, and initiating patient support programs to help patients learn to use these software-based therapeutics.
PREDICTION #6: Clinical trial sponsors will drive a new framework for DCT technology and services (rather than the other way around)
Even with nearly nine in 10 sponsors saying they will use some elements of DCT technologies in their trials, we still have a lot to learn. We’ll continue to see a lot of experimentation in trying to understand the most effective new methods, technologies, and processes for designing and executing DCTs and improving various aspects of clinical research. But, with business models in flux and an uncertain economy, we’ll see more disruption in the DCT software space, as technology providers pivot to meet industry needs.
For instance, technology providers will work to resolve the complexities of DCT software integration, and drill down to solve specific trial problems rather than offer ‘end all be all’ solutions to sponsors that prefer a hybrid approach. Until recently, the progress of DCTs has been largely driven by providers – often, working in a bubble without collaborating closely with trial sponsors.
In 2023, sponsors will take the lead. Rather than technology providers dictating what their product/services can do to improve clinical research, sponsors will seek technology providers that solve their specific challenges. As they become more researched and familiar with DCT technologies, sponsors will define what trial improvements are required, and successful technology manufacturers will pivot accordingly.
PREDICTION #7: Next year, decentralized and hybrid clinical trials will become simply “clinical trials”

The decentralized clinical trial (DCT) model works and works well. It’s no longer a leap of faith, as a 2022 study from the Tufts Center for the Study of Drug Development shows that DCTs can achieve net financial benefits ranging from five to 13 times for Phase II and Phase III trials, equating to roughly $10 million and $39 million ROI, respectively. COVID-19 made DCTs a necessity. Positive returns will make DCTs the de-facto standard.
Expect 2023 to be a pivotal year, capping a year or more of strong growth2 in decentralized and hybrid clinical trial deployment. The next evolution of DCTs will involve self-service tools that enable sponsors and sites to deploy and operate global studies on a common platform using standardized processes. We see evidence of this pivot from customers and partners who aim to leverage digital tools across their pipeline. The industry is no longer dipping their toes in the DCT water; rather, leading pharmaceutical companies like GSK and AstraZeneca, are expanding its use.2, 3
We are living the evolution of clinical trials – similar to how consumers migrated to online banking without even realizing that a major shift was taking place in their everyday lives. Sponsors, sites, and patients will expect digital tools to drive clinical trial performance, superior experience, greater diversity, and better outcomes.
Sources:
- The DHC Group, “The State of Omnichannel HCP Engagement in Pharma,” (November 2022).
- 2022 forecast: decentralised trials to reach new heights with 28% jump, https://www.clinicaltrialsarena.com/analysis/2022-forecast-decentralised-trials-to-reach-new-heights-with-28-jump/
- https://www.astrazeneca.com/r-d/digital-health-revolutionising-healthcare-for-patients.html
- https://www.businesswire.com/news/home/20220907005594/en/Medable-Selected-by-GSK-to-Power-Decentralized-and-Hybrid-Clinical-Trials-Across-Global-Product-Portfolio
Curavit’s crystal ball – how will 2023 drive meaningful changes in clinical research
December 22, 2022

The life sciences industry is flexing towards innovation in new areas, faster than ever before, and increasing patient care in astonishing ways. Decentralised oncology trials, for example, have shown actual predictive outcome value. We can now measure patient activity, steps, and movement continuously and in real time, which serves as a new potential indicator of treatment effectiveness.1 And, digital therapeutics have emerged as an effective treatment for chronic diseases, including mental illness. The rapid innovation is both exciting and disruptive, so it’s important to strategise accurately for what we can expect in the year ahead.
Prediction 1: the FDA will become more directive and collaborative on guidelines for DCTs.
Traditional protocol designs are built upon years of empirical evidence and consensus among highly rated peer reviewed journals. For new decentralised approaches, this is practically non-existent. This will lead to more pre-protocol design discussions between sponsors and CROs and regulatory bodies seeking input on new and potentially acceptable approaches to, for example, measure digital endpoints. The risk of not having these discussions is to conduct expensive trials only to discover too late that they were measuring the wrong endpoint, in the wrong way, or with a tool or technology the FDA does not accept.
Curavit is currently conducting a decentralised trial for a digital therapeutic that began with discussions with the FDA. In this case, the indication was well-known, treated for decades by traditional medical interventions, and copious peer reviewed data to call upon. However, since the route of administration itself was new – i.e., digital rather than in pill form – all stakeholders recognised how crucial it would be to involve the FDA early and often. Specifically, they discussed which patient survey format would be best, which scores to include or exclude, and acceptable means of data capture.
As this collective body of experience continues to proliferate, 2023 will see additional FDA guidance. It is likely that the FDA will address various elements associated with DCTs more granularly than ever. These may include best practices for measuring digital endpoints, biomarkers, and telemedicine and ePRO (Patient Reported Outcomes), as well as risk factors most concerning to the FDA. For instance, at a recent presentation to the Society of Quality Assurance 2022 Annual Meeting, the FDA Office of Regulatory Affairs Bioresearch Monitoring Division Director Anne Johnson emphasised that DCTs are largely reliant on electronic data integrity and therefore subject to firmly established 21 CFR Part 11 compliance.2
Prediction 2: More clinical trial services will become remote, beyond just patient monitoring.
We will see continued increases in remote clinical trial activities and services in 2023, such as remote monitoring, remote site staff training, remote site activation visits, remote quality management meetings, remote safety management meeting,s and more.
These unprecedented clinical trial activities represent a fundamental shift that is still unfolding. There was a time when Source Data Verification (SDV) by any other means than frequent and extremely costly on-site CRA visits was unthinkable. We now see continuing proof points that conducting SDV remotely can not only save time and travel costs, but can also increase quality.
Curavit recently worked on a 28-site, US-based trial where more than half of the source data verification was conducted remotely with secure, remote access to the eTMF and EDC systems. Instead of using generalised, on-site CRAs, Curavit’s therapeutic area specialists handled this significant task from afar, prioritising specific expertise over physical proximity. This had a significant impact on data quality and speed, as well as reductions in travel and costs. Curavit was also able to conduct additional Q/C measures simultaneously, which otherwise would have been a separate process.
Prediction 3: AI innovation will expand its application to enhance patient experience.
Although “Enquire Here” buttons are common for large patient enrolment providers, recent advances in Natural Language Processing (NLP) – a form of artificial intelligence or AI – allow for far greater, more meaningful, and effective patient engagement. Technologies such as BERT3 and GPT-3 catapult NLP capabilities beyond basic processing, into the realm of language intelligence. Potential applications will surpass current-day screening chat bots, which automate FAQ workflow and are only capable of answering the most basic patient questions.
In 2023, expect to see AI innovations improve enrolment agility and, most importantly, the patient experience in a clinical trial. For instance, NLP will respond to patient concerns or enquiries with more humanised responses and alert clinicians faster and automatically. This will, in turn, improve patient interest, trust, engagement, enrolment, and clinical trial retention. In addition to patient benefits, AI will enable actionable real-time metrics and analysis and a near-immediate feedback loop on the investigational drug’s impact on patients’ daily lives.
Prediction 4: digital therapeutics companies will focus on the difficult last mile to commercialisation.
Historically, digital therapeutics (DTx) companies have directed about 95% of their effort into gaining FDA approval and 5% into market access strategy. In 2023, this will shift to a 60%/40% split, with DTx companies having an earlier focus on the commercialisation process, while simultaneously working toward earning FDA approval.
This ’last mile’ is completely unchartered territory for DTx companies. They face new obstacles bringing their therapeutics to market – for example, physicians’ lack of awareness of the DTx and their inability to easily prescribe them. There are still many unknowns around getting DTx products on the formulary and how to prescribe them to patients – doctors can’t just write a prescription and send patients off to the local drugstore when prescribing the use of an app.
And, whereas traditional drug companies may spend up to $300 million to launch a product, most DTx startups don’t have the budget to spend on commercialisation strategies such as building a field team, equipping marketing teams with supporting analytics technology, and initiating patient support programs to help patients learn to use these software-based therapeutics.
Beyond 2023 – the Sovereign Patient ID
The concept of patients owning their own data has been around since the advent of electronic health records. However, 2023 will see new technologies such as blockchain and smart contracts bring the Sovereign Patient ID concept closer to reality. This will give the patient the ability to own their own identity and associated data on their own devices, as opposed to their identity being created and stored separately by each service provider: a state of error prone, redundant inefficiency. The life sciences industry will collaborate and share lessons learned with other verticals that are currently exploring the same concept, such as “Self-Sovereign Identity” (SSI).4
This problem will not be solved in 2023, but progress will be made.
References
1. Gresham G, Hendifar AE, Spiegel B, Neeman E, Tuli R, Rimel BJ, Figlin RA, Meinert CL, Piantadosi S, Shinde AM. Wearable activity monitors to assess performance status and predict clinical outcomes in advanced cancer patients. NPJ Digit Med. 2018 Jul 5;1:27. doi: 10.1038/s41746-018-0032-6. PMID: 31304309; PMCID: PMC6550281.
2. Chapman, J. An FDA Perspective on Decentralized Clinical Trials: Part 1. July 28, 2022.
3. Devlin, J, Chang, M.W. Open Sourcing BERT: State of the Art Pre-Training for Natural Language Processing. November 2, 2018.
4. Preukschat, A., Reed, D. Self-Sovereign Identity- Decentralized Digital Identity and Verifiable Credentials. Manning. 2021.
About the Author
 Dr. Pam Diamond is co-founder and chief medical officer of Curavit, a virtual contract research organisation (VCRO) that designs and executes decentralised clinical trials. She is a board-certified, Boston-based otolaryngologist/head and neck surgeon who was affiliated with Harvard Medical School (HMS) and Massachusetts Eye and Ear Infirmary (MEEI) for over 30 years. At Curavit, Dr. Diamond provides medical and scientific expertise and oversight to the design and execution of Curavit’s decentralised clinical trials. She received her medical degree from the University of Rochester School of Medicine and completed her otolaryngology/head and neck surgery residency at Harvard Medical School/MEEI.
Dr. Pam Diamond is co-founder and chief medical officer of Curavit, a virtual contract research organisation (VCRO) that designs and executes decentralised clinical trials. She is a board-certified, Boston-based otolaryngologist/head and neck surgeon who was affiliated with Harvard Medical School (HMS) and Massachusetts Eye and Ear Infirmary (MEEI) for over 30 years. At Curavit, Dr. Diamond provides medical and scientific expertise and oversight to the design and execution of Curavit’s decentralised clinical trials. She received her medical degree from the University of Rochester School of Medicine and completed her otolaryngology/head and neck surgery residency at Harvard Medical School/MEEI.
Digital Therapeutics: From Product Development and Approval to Commercialization and Reimbursement
As seen on – Today’s Clinical Lab
December 12, 2022
Estimates of the US digital therapeutics (DTx) market have jumped by billions each year since 2019 and, as of November 2022, is expected to hit $11.2 billion by 2030, while the global DTx market is projected to reach $56 billion over the next five years. The market was driven by the FDA fast-tracking pandemic-related approvals for prescription DTx products to help treat the sharp increase in patients with anxiety and depression.
There are many types of DTx manufacturers, ranging from emerging DTx companies to public companies like Pear Therapeutics and Akili Interactive to global pharmaceutical companies like Roche and AstraZeneca, which are acquiring or partnering with DTx startups to enter the market.
To add further complexity, there are FDA-approved prescription digital therapeutics, nonprescription digital therapeutics, and those that may eventually seek approval.
Benefits of digital therapeutics for trial recruitment
Traditional clinical trials are complex, but architecting a DCT from the ground up is even more complicated. And while nearly nine in 10 sponsors say they use some elements of DCT technologies in their trials, fully virtual trials are still rare. At a recent conference, one top-10 pharma executive said that while more than half of their trial site visits are virtual, no trials are 100 percent virtual.
One reason for this is because designing a DCT protocol requires highly specialized expertise. Sponsors are leaning into the decentralized approach to speed patient recruitment, increase access and diversity, improve efficiency, and capture real-world data, but are still developing protocol designs within a traditional framework. Expert DCT protocol designers, however, review trial designs to determine what aspects can be decentralized (and which cannot) and the best way to decentralize those elements. They factor DCT considerations into the process from the beginning, instead of shoehorning digital elements into the trial later or superimposing them over traditional designs.
Swing Therapeutics is a DTx company that was founded less than three years ago with $9 million in seed funding and that wrapped up $10.3 million in Series A funding in June. The company is running a hybrid trial of its investigational DTx for fibromyalgia and is expected to enroll up to 300 participants recruited from 15–25 physical sites, plus a virtual site.
The virtual site provider is remotely recruiting, screening, consenting, and enrolling participants in Swing’s PROSPER-FM trial from across the US.
By eliminating physical and geographic barriers to trial participation and execution, they have improved patient enrollment by 10x. In fact, the virtual site has surpassed all the bricks-and-mortar sites in patient enrollment.
Decentralized clinical trials are well-suited for studying digital therapeutics
Many virtual or decentralized clinical trial (DCT) specialists are successful in supporting DTx companies, as DCTs are well-suited to support prescription and non-prescription DTx studies. Fundamentally, there are no physical logistics with a DTx—no shipping, storing, chain of control, cold storage, or biohazards, and endpoints can often be captured within the DTx application itself, naturally aligning DCTs with DTx studies. Ultimately, Swing hopes for FDA-approval and will go to market.
“We are focused on getting patient recruitment right,” says Mike Rosenbluth, PhD, chief executive officer at Swing. “A virtual services model enables us to efficiently recruit participants representative of the entire patient population. It solves a huge challenge and will be critical to rapidly develop the evidence needed to bring an effective digital therapy to millions suffering from chronic illness.”
Ongoing challenges of commercializing digital therapeutics
And, while the research and development processes involved in digital therapeutics are innovative, commercializing a DTx may require more out-of-the-box thinking. Many presenters at the fall DTx East event said that even after successfully earning FDA-approval, their therapeutics are failing in the marketplace. There are new challenges to address such as lack of awareness by clinicians and their inability to easily prescribe DTx to patients.
This last challenge is uncharted territory for DTx companies. And whereas traditional drug companies average between $200–$300 million to launch a product, most DTx companies don’t have that kind of funding available to them. Plus, there are various launch challenges, patient support programs to implement, and sales and marketing teams to recruit and train.
For Swing Therapeutics and other DTx companies to be profitable or even sustainable, they need to make it easy for clinicians to prescribe digital therapeutics and get reimbursed, while also making it easy for patients to use DTx.
A new CMS code that went into effect in April 2022 will help by making it easier for commercial and Medicaid plans to cover these therapies. Yet, there are still many questions about what payment models will work best and how to get on formularies and more.
Virtual CRO Curavit raises $5m to grow digital therapeutics clinical trial business
Media Coverage | Outsourcing Pharma
November 23, 2022

Virtual CRO Curavit Clinical Research has tapped investors for cash, securing $5 million in series A funds to support its targeting of the digital therapeutics space.
Can pharma prop up the digital health recession?
Media Coverage | Digital Health
November 21, 2022

Investors and buyers say pharma-related technologies are piquing their interest even within a tumultuous economy.
While the digital health ecosystem is anticipating a massive reset in 2023, pharmaceutical companies are willing to invest in clinical trial technology and digital therapeutics. Also, retail companies like CVS and Walgreens and payers are interested in pharma-related innovations. All this presents a potentially big opportunity for digital health investors and companies alike, experts say.
“One segment that is still eager to spend is pharma, particularly on the clinical trials sector” said Dr. Sunny Kumar, a partner at the venture capital firm GSR Ventures. According to the Digital Health Business & Technology database, companies focused on digital health trial technology have raised nearly $165 million this year across nine deals, including a $5 million investment into virtual research organization Curavit last Tuesday.
GSR’s portfolio companies include Medable, one of the industry’s biggest decentralized trial technology companies that received $304 million in funding last October. Kumar said companies like this have a tightly aligned incentive structure. “No one is truly recession proof, but companies in that space are still getting [interest] because they’re bringing a certain value proposition to the table. They’re decreasing clinical trial time and bringing drugs to market faster,” he said.”
Dr. Justin Norden, also a partner at GSR Ventures, said he prefers companies that sell to the pharma sector.
“Pharma makes decisions faster for bigger contracts with research and development focused on a return of investment,” Norden said. “If you’re a digital health company that’s going to monetize with pharma, it’s going to be a faster and easier path.”
Scott Barclay, managing director at venture capital firm Insight Partners, has invested in Trialjectory, an AI based trial matching platform that uses self-reported clinical information to facilitate clinical trial search, matching and enrollment. The company raised $20 million in a Series A round in February.
“We need to bring software and appropriate data liquidity to trials,” Barclay said. “Trials need to be better, faster, more expansive and more inclusive.”
Digital therapeutics is another area of potential investment for pharma companies, particularly as payers are increasingly willing to cover them. At the HLTH conference held last week in Las Vegas, Teva Pharmaceuticals said it was partnering with HealthTap, a virtual care management company, to expand its digital health platform. Manny Montalvo, head of digital health and innovation at Teva, said technology partnership is vital to its overall strategy on digital.
“We’re always looking to collaborate whether it’s plugging into an [electronic medical record] system, directly ordering online or something else,” Montalvo said. “If someone has better software than we do, we’re always looking to build off the platform that we have.”
Disruption in pharma is also coming from the retail side, experts say. Both CVS Health and Walgreens are investing in different technologies to create more efficient operations, including entering the de-centralized clinical trial space. Rina Shah, Walgreens’ vice president of the pharmacy of the future, said the company is also using technology to improve fulfillment, prescription renewals and medication adherence.
“Technology and analytics really drive the core infrastructure of how we deliver care all the way,” Shah said. “Our micro fulfillment center is primarily driven by technology and automation. We’re able to fulfill hundreds of thousands of prescriptions with the oversight of a pharmacist and technician onsite.”
It also has invested heavily in technology in terms of how it engages with patients. Shah said it works with both payers and providers to use “behind the scenes data” that helps the retail company better understand the patients needs.
In the area of improved pharma operations, Paul Markovich, CEO of Blue Shield of California, said the health insurance company aims to use technology to improve the pharmacy value chain. The pharma value chain is the process in which medications go to market. Companies like Blue Shield of California play an integral role as the ones who reimburse for these medications.
“We’ve laid out a vision for what a more efficient, consumer-centered pharma value chain will look like, but you’ve got to do it at scale,” Markovich said. “We’ve gone through a request for proposal but we’re still in the middle of trying to figure out which vendors could fit with our vision.”
Curavit Clinical Research Raises $5 Million led by Osage Venture Partners
Media Coverage | The Business Journals
November 18, 2022

This week’s Lab Notes has reports on a cancer research collaboration, a biotech startup’s multimillion-dollar seed funding round, a local firm’s investment in a virtual contract research organization and more
Curavit Raises $5 Million in Series A Funding to Accelerate Growth in Digital Therapeutics Clinical Research
November 14, 2022

Industry’s first virtual CRO that specializes in decentralized clinical trials achieves key milestones
PHILADELPHIA and NEW YORK, Nov. 14, 2022 /PRNewswire/ — Curavit Clinical Research, a virtual contract research organization (VCRO) that specializes in decentralized clinical trials (DCTs), today announced it raised $5 million in Series A funding to accelerate its growing portfolio of research in the global digital therapeutics (DTx) market (projected to grow at a CAGR of 31.4% through 2026). The new funding will be used to expand the company’s DCT capabilities, partnerships, and market adoption of Curavit’s virtual CRO services and platform for prescription and non-prescription digital therapeutics trials.
The funding was led by early-stage technology investor Osage Venture Partners with additional investment from Royal Street Ventures and Narrow Gauge Ventures. It adds to early investments from Curavit founders and individual investors, including industry veterans Clark Golestani, former president of emerging businesses and global CIO of Merck, and former president and co-founder of Veeva Systems, Matt Wallach.
“In order to dramatically lower the cost and increase the speed of clinical trials, the industry must take a new, digital-first approach,” said Wallach who serves on Curavit’s board of advisors. “Curavit was founded by seasoned veterans with deep experience in that sweet spot where technology innovation meets process excellence so I’m proud to play a part in their journey to improve clinical trials.”
“This is an important milestone for Curavit and the industry’s continued momentum in digital therapeutics and decentralized approaches to clinical research,” said Joel Morse, co-founder and CEO of Curavit. “Traditional trial processes and timelines are insufficient – and they limit patient participation. New digital therapeutics are ideally suited for a DCT approach and will help improve access and drive new unique therapies to patients faster.”
The funding brings Curavit’s total capital raised to more than $8 million. Curavit has more than doubled its revenue in 2020 and 2021 and is on the same pace this year. More than half of its customer base are emerging digital therapeutics companies whose clinical research needs align with Curavit’s focus on virtual site services and DCT expertise.
“We are pleased to partner with Curavit on the next phase of their journey,” said Nate Lentz, Managing Partner at Osage Venture Partners. “The COVID-19 pandemic and rapid growth of digital therapeutics has driven a new digital model, where clinical trials are increasingly decentralized and require a new combination of technologies, services, and expertise not available in the marketplace. Curavit’s team and offering are well-positioned to fill this void and become the leading virtual CRO.”
Since its founding in late 2019, Curavit has accomplished key successes on its mission to bring clinical trials of innovative therapies to more patients in the cloud, including:
- Support for important research with digital therapeutics companies, including Swing Therapeutics, Lark Health, Curio, and Sana.
- Strategic partnerships with life sciences digital technology and data providers, including Ripple Science, for its direct-to-patient software platform; ixlayer, to provide easy access to clinical-grade diagnostic lab testing in DCTs; and 1nHealth, for digital patient recruitment and enrollment.
- Hired experienced industry leaders in top positions including Jay Collier as COO, Candice Del Rio as director of clinical operations, and Chris O’Shaughnessy as VP of business development.
In other news, Curavit joined the Digital Therapeutics Alliance, whose aim is to broaden the understanding, adoption, and integration of clinically evaluated digital therapeutics with patients, clinicians, payors, policymakers through education, advocacy, and cross-industry collaboration.
Osage Venture Partners (OVP) is a venture capital firm located just outside of Philadelphia, PA. It partners with exceptional entrepreneurs, building the next generation of leading B2B software and tech-enabled services companies. OVP has consistently focused on this strategy since its inception in 2005, making over sixty investments in early-stage B2B companies over that time. For more information, visit OsageVenturePartners.com.
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
View original content to download multimedia:https://www.prnewswire.com/news-releases/curavit-raises-5-million-in-series-a-funding-to-accelerate-growth-in-digital-therapeutics-clinical-research-301675207.html
SOURCE Curavit Clinical Research
Curavit Raises $5 Million in Series A Funding to Accelerate Growth in Digital Therapeutics Clinical Research
Media Coverage | Trial Site News
November 14, 2022

Curavit Clinical Research, a virtual contract research organization (VCRO) that specializes in decentralized clinical trials (DCTs), today announced it raised $5 million in Series A funding to accelerate its growing portfolio of research in the global digital therapeutics (DTx) market (projected to grow at a CAGR of 31.4% through 2026). The new funding will be used to expand the company’s DCT capabilities, partnerships, and market adoption of Curavit’s virtual CRO services and platform for prescription and non-prescription digital therapeutics trials.
Curavit reaps $5M in series A funding to fuel decentralized trial growth
Media Coverage | HIT Consultant
November 14, 2022

What You Should Know:
– Curavit Clinical Research, a virtual contract research organization (VCRO) that specializes in decentralized clinical trials (DCTs) announced it raised $5M in Series A funding to accelerate its growing portfolio of research in the global digital therapeutics (DTx) market. The round was led by Osage Venture Partners with additional investment from Royal Street Ventures and Narrow Gauge Ventures.
– The new funding will be used to expand the company’s DCT capabilities, partnerships, and market adoption of Curavit’s virtual CRO services and platform for prescription and non-prescription digital therapeutics trials.
In addition, Curavit joined the Digital Therapeutics Alliance, whose aim is to broaden the understanding, adoption, and integration of clinically evaluated digital therapeutics with patients, clinicians, payors, policymakers through education, advocacy, and cross-industry collaboration.
Curavit Background
Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations
Curavit reaps $5M in series A funding to fuel decentralized trial growth
Media Coverage | Fierce Biotech
November 14, 2022

The funding round was led by Osage Venture Partners with additional investments by Royal Street Ventures and Narrow Gauge Ventures, the company said in a Nov. 14 press release. To date, the company has raised more than $8 million.
The money is expected to support Curavit’s expansion of decentralized clinical trial offerings, partnerships and adoption of its CRO services and platform for prescription and non-prescription digital therapeutics trials. The company cited estimates the global digital therapeutics market will experience growth of 31.4% by the end of 2026.
“Traditional trial processes and timelines are insufficient and they limit patient participation,” Joel Morse, co-founder and chief executive of Curavit, said in the press release. “New digital therapeutics are ideally suited for a DCT approach and will help improve access and drive new unique therapies to patients faster.”
RELATED
Curavit launched in late 2019, just months before the onset of the COVID-19 pandemic. Disruptions caused by the crisis initiated a global embrace of decentralized clinical trials that have become more the norm than exception.
The company also said more than half of its customer base are companies focused on emerging digital therapeutics that pair with virtual site services and decentralized clinical trial experience.
Curavit Raises $5 Million in Series A Funding to Accelerate Growth in Digital Therapeutics Clinical Research
Media Coverage | Business Insider
November 14, 2022

Industry’s first virtual CRO that specializes in decentralized clinical trials achieves key milestones
PHILADELPHIA and NEW YORK, Nov. 14, 2022 /PRNewswire/ — Curavit Clinical Research, a virtual contract research organization (VCRO) that specializes in decentralized clinical trials (DCTs), today announced it raised $5 million in Series A funding to accelerate its growing portfolio of research in the global digital therapeutics (DTx) market (projected to grow at a CAGR of 31.4% through 2026). The new funding will be used to expand the company’s DCT capabilities, partnerships, and market adoption of Curavit’s virtual CRO services and platform for prescription and non-prescription digital therapeutics trials.
Curavit, the industry’s first virtual CRO that specializes in decentralized clinical trials reaches key milestones.
The funding was led by early-stage technology investor Osage Venture Partners with additional investment from Royal Street Ventures and Narrow Gauge Ventures. It adds to early investments from Curavit founders and individual investors, including industry veterans Clark Golestani, former president of emerging businesses and global CIO of Merck, and former president and co-founder of Veeva Systems, Matt Wallach.
“In order to dramatically lower the cost and increase the speed of clinical trials, the industry must take a new, digital-first approach,” said Wallach who serves on Curavit’s board of advisors. “Curavit was founded by seasoned veterans with deep experience in that sweet spot where technology innovation meets process excellence so I’m proud to play a part in their journey to improve clinical trials.”
“This is an important milestone for Curavit and the industry’s continued momentum in digital therapeutics and decentralized approaches to clinical research,” said Joel Morse, co-founder and CEO of Curavit. “Traditional trial processes and timelines are insufficient – and they limit patient participation. New digital therapeutics are ideally suited for a DCT approach and will help improve access and drive new unique therapies to patients faster.”
The funding brings Curavit’s total capital raised to more than $8 million. Curavit has more than doubled its revenue in 2020 and 2021 and is on the same pace this year. More than half of its customer base are emerging digital therapeutics companies whose clinical research needs align with Curavit’s focus on virtual site services and DCT expertise.
“We are pleased to partner with Curavit on the next phase of their journey,” said Nate Lentz, Managing Partner at Osage Venture Partners. “The COVID-19 pandemic and rapid growth of digital therapeutics has driven a new digital model, where clinical trials are increasingly decentralized and require a new combination of technologies, services, and expertise not available in the marketplace. Curavit’s team and offering are well-positioned to fill this void and become the leading virtual CRO.”
Since its founding in late 2019, Curavit has accomplished key successes on its mission to bring clinical trials of innovative therapies to more patients in the cloud, including:
- Support for important research with digital therapeutics companies, including Swing Therapeutics, Lark Health, Curio, and Sana.
- Strategic partnerships with life sciences digital technology and data providers, including Ripple Science, for its direct-to-patient software platform; ixlayer, to provide easy access to clinical-grade diagnostic lab testing in DCTs; and 1nHealth, for digital patient recruitment and enrollment.
- Hired experienced industry leaders in top positions including Jay Collier as COO, Candice Del Rio as director of clinical operations, and Chris O’Shaughnessy as VP of business development.
In other news, Curavit joined the Digital Therapeutics Alliance, whose aim is to broaden the understanding, adoption, and integration of clinically evaluated digital therapeutics with patients, clinicians, payors, policymakers through education, advocacy, and cross-industry collaboration.
About Osage Ventures
Osage Venture Partners (OVP) is a venture capital firm located just outside of Philadelphia, PA. It partners with exceptional entrepreneurs, building the next generation of leading B2B software and tech-enabled services companies. OVP has consistently focused on this strategy since its inception in 2005, making over sixty investments in early-stage B2B companies over that time. For more information, visit OsageVenturePartners.com.
About Curavit
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
View original content to download multimedia:https://www.prnewswire.com/news-releases/curavit-raises-5-million-in-series-a-funding-to-accelerate-growth-in-digital-therapeutics-clinical-research-301675207.html
SOURCE Curavit Clinical Research
Curavit Clinical Research raised $5 million in Series A funding
Media Coverage | FORTUNE – Term Sheet Newsletter
November 14, 2022
Curavit Clinical Research, a Scarsdale, N.Y.-based virtual contract research organization company, raised $5 million in Series A funding. Osage Venture Partners led the round and was joined by investors including Royal Street Ventures and Narrow Gauge Ventures.
More Than One Way to Crack a Walnut: Four Fundamental Components of a Successful Decentralized Clinical Trial
As seen on – Drug Information Association
November 8, 2022
There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
1. Expert Protocol Design Review: What Can Be Decentralized?
Traditional clinical trials are complex, but architecting a DCT from the ground up is even more complicated. And while nearly nine in 10 sponsors say they use some elements of DCT technologies in their trials, fully virtual trials are still rare. At a recent conference, one top-10 pharma executive said that while more than half of their trial site visits are virtual, no trials are 100 percent virtual.
One reason for this is because designing a DCT protocol requires highly specialized expertise. Sponsors are leaning into the decentralized approach to speed patient recruitment, increase access and diversity, improve efficiency, and capture real-world data, but are still developing protocol designs within a traditional framework. Expert DCT protocol designers, however, review trial designs to determine what aspects can be decentralized (and which cannot) and the best way to decentralize those elements. They factor DCT considerations into the process from the beginning, instead of shoehorning digital elements into the trial later or superimposing them over traditional designs.
The best resources are experienced in clinical research, the therapeutic area of the trial, and DCT technologies. These experts know how to allocate the right DCT resources to allow for maximum patient flexibility during the trial. For instance, a lot of calendaring is often involved in planning a DCT since the patient is not tied to a specific location. It becomes critical to ensure that there are enough calendar slots for televisit appointments at optimum times for patients. A DCT protocol design expert will take all resource considerations into the design, thinking ahead about what can be done by a coordinator instead of by a clinician or registered nurse and other ways to optimize staffing.
2. Patient Solicitation Partners: Recruit, Screen, Consent, Enroll
Patient recruitment is notoriously time-consuming, but many technology-enabled firms leverage solutions specifically for a DCT. For example, one patient recruiting firm targets potential patients on digital channels using sophisticated targeting, patient-centric recruitment, and technology. Once a patient clicks on an ad, they are taken to a self-service landing page with more info about the trial and self-screening questions. If the patient passes, they can immediately schedule a live screening call, eConsent, and enroll in the trial.
One virtual CRO specializing in DCTs collaborated with this patient recruiting firm on a trial of an investigational DTx for chronic cardiovascular disease. Through targeted ads on key digital channels (i.e., Google, Reddit, Facebook, Instagram), the CRO recruited 50 patients in 10 days, surpassing the sponsor’s originally estimated four-week timeline. In addition, 39 percent of patients who clicked on an ad completed the pre-screen form – again, beating a projected 24 percent completion rate. In total, the CRI and the patient recruiting firm recruited, consented, and enrolled 150 patients in just 58 days.
“Most recruitment methods miss opportunities to enroll patients, whether in finding the right people or communicating the opportunity correctly. Expert recruitment processes coupled with technology-activated enrollment at the site and CRO levels fill trials faster with less friction,” said Dan Brenner, CEO and founder of the patient recruiting firm. “Digital recruitment allows more patients to be enrolled in the right trials, seamlessly. It breaks down the barriers between patients and studies, increasing access for more patients.”
One independent software company optimizes the use of data to digitally recruit, screen, and consent patients in DCTs. With access to 350 million lives of anonymized medical records globally, and 200 million lives of anonymized claims data in the US, the firm uses a data science-based approach to target patients across a large geography.
“In DCTs, there’s a longer-term opportunity to marry enrollment and operational data to continuously learn and refine the patient recruitment and enrollment process,” said Matt Walz, its CEO. “How else can we use this data to improve trials? For instance, this data could inform protocol development so that sponsors can better assess how inclusion/exclusion criteria might impact enrollment. All this data can improve how we work with patients.”
In the end, whichever partner supports the enrollment process, data must be aggregated on a single platform for a seamless site and patient experience, and as an opportunity for continuous improvement. “DCTs expand access to patients who live a distance from academic centers, but they can also add burden,” Rosenberg continued. “For instance, patients must decide about each visit: Does someone come to their house, do they stop at a CVS [pharmacy], or go to the clinic? It is important to consider the impact of this new experience on patients. DCT technology enables us to survey patients in real time and then find ways to alleviate any unforeseen issues.”
3. Remote Data Capture Tools: From Clinical-Grade Sensors to ePROs
The global remote patient monitoring market is projected to be worth over $1.7 billion by 2027, up 128 percent from 2021, and the increased use of a decentralized approach could push those numbers higher as DCTs require clinical-grade medical devices. Hundreds of devices already exist that capture digital biomarkers including sleep patterns, heart rate, and blood pressure. For example, continuous glucose monitors remind diabetes patients to take their insulin while allowing clinicians to monitor their disease.
In addition to these remote medical devices, DCTs can now incorporate convenient, remote lab testing with an end-to-end health testing platform. By making health testing easy for patients in a DCT, specialized firms help sponsors improve completion rates and likelihood of patient retention for the duration of the trial. One CRO partnered with such a firm for a fully decentralized trial for an investigational digital therapeutic for fibromyalgia. The firm’s health testing solution helped speed enrollment for the 12-week trial by 10 times over a traditional trial model.
“Lab testing is an integral part of most clinical trials but can compound patients’ burden in traditional settings,” explained Pouria Sanae, the firm’s CEO and co-founder. “We reduce friction for patients and sponsors by simplifying the process and streamlining data collection on the back end for DCTs.”
Electronic patient-reported outcomes (ePROs) are another critical remote data capture tool frequently used in DCTs. Look for a partner that is focused on ensuring a frictionless patient experience.
“In a DCT, patients have a larger responsibility to report their experiences even if they can do it remotely. At the same time, there is less in-person bonding where the clinician can get to know the patient’s everyday user experience. That is why it is so important to provide them with not only intuitive interfaces, but also concierge-like support throughout the trial,” Rosenberg explained.
4. Single DCT Platform: Bringing It All Together in the Cloud
So many moving parts in a DCT make it imperative to have a single platform that brings them all together for streamlined data analysis and visibility. “All DCT stakeholders need to have visibility into the entire trial journey and connect into the same system,” added Walz. “We need to provide a single entry point to trial technology regardless of recruitment source for a consistent patient experience and streamlined login for sites.”
An ecosystem of pre-vetted partners with technologies that easily integrate into a single platform can also give sponsors the confidence they need to dip their toes into the DCT pool while saving significant up-front time and money managing complex integrations. Many partnering companies and products have pre-built connectors for industry-leading DCT platforms which can drastically reduce start-up time. For instance, one CRO and its partners have reduced DCT start-up time from 14 to six weeks.
DCTs offer sponsors unparalleled trial flexibility, which is exciting in its optionality but can complicate trial design. Rather than being paralyzed by choice, start with these four fundamental elements, build from there, and remember that there is always more than one way to crack a walnut.
Tips for tackling trial recruitment and retention woes in oncology
October 31, 2022
How new tools are helping companies find and keep cancer patients in clinical studies.
Oncology treatment is improving at a rapid clip, so for people with advanced cancer, a clinical trial may offer new hope when other options have fallen short. But cancer patients still aren’t signing up — a problem that has vexed the industry for years. It’s estimated that fewer than 5% of cancer patients participate in clinical trials, most of them after they have already tried another treatment first.
But trial participation can bring rewards. A study in the Journal of the National Comprehensive Cancer Network found that while only 0.01% of the 12 million patients in the National Cancer Database enrolled in a clinical trial as a first-line treatment option, those that did had better outcomes than non-participants, although they also tended to be younger and healthier than the typical cancer patient.
To help more patients take advantage of these opportunities, organizations are testing new technological tools and focusing on convenience to boost enrollment and retention, as well as diversity.
Barriers to participation
One of the primary reasons cancer patients don’t enroll in clinical trials is perhaps the most obvious — they’re unaware trials exist, said Dr. Arturo Loaiza-Bonilla, co-founder and chief medical officer of Massive Bio, a New York City-based technology company using an AI-driven platform to match oncology patients with clinical trials.
Dr. Arturo Loaiza-Bonilla, co-founder and chief medical officer, Massive Bio Permission granted by Dr. Arturo Loaiza-Bonilla
“Most patients don’t have any idea what their options are,” he said. Even when a patient is interested in participating in research, determining which trial is right for them is often a substantial hurdle. Oncologists often don’t have the time to pore through options to find the right match. It can easily take up to an hour to go through all the criteria and data to search for a trial for one patient, Loaiza-Bonilla said. Some larger practices may have research coordinators to navigate this process, “but in a community practice, you don’t have that luxury, (and) you don’t have that person or expertise,” he said.
Oncology trials typically require patients to meet very restrictive participation parameters, ranging from the genetics of their cancer to the type of treatments they’ve previously undergone.
“Getting into a clinical trial for oncology is extremely challenging because there are so many criteria required,” Loaiza-Bonilla said.
Finding the right match takes an intensive approach, and as a result, many patients miss out.
“It has to be almost like a real-time activation for the patient. And if there’s no system to do it in real time for you, no one’s going to help you,” he said.
There are also emotional challenges and logistical barriers to contend with, said Candice Del Rio, director of clinical operations for Curavit, a virtual CRO that operates decentralized clinical trials. When a patient receives a cancer diagnosis, they are already overwhelmed, which may make them reluctant to take on additional treatments. She saw this firsthand as a nurse working with participants in oncology clinical trials. For patients still processing that initial shock, the idea of participating in research may seem like an additional burden.
“They may say, ‘Look, I just got to the hospital. I’m overwhelmed. I just need some downtime. I don’t know that I want to do anything extra. I just kind of want to stay the course,’” Del Rio said.
Organizations need to take steps to address these barriers if they want to increase enrollment.
Strategies to boost enrollment
Massive Bio is tackling the problem by enlisting tools to help patients more easily find the right trial.
“We founded the company with the goal of making clinical trials accessible for all cancer patients no matter where they are, and using technology at scale to make it work,” said Loaiza-Bonilla. “The space is already crowded by a lot of people saying we’re going to try to solve the problem, but there’s no good engine that’s able to connect the dots, and that’s what we’re aiming for with the company.”
Massive Bio’s AI-driven technology, the Deep Learning Clinical Trial Matching System (DLCTMS), pairs patients with existing trials in the ClinicalTrials.gov national database by combing through medical records to find the most clinically appropriate options based on the specifics of their cancer, including biomarker data. The company’s platform, which has onboarded 100,000 cancer patients to date, also includes other factors in its algorithm, such as the trial location, the patient’s insurance coverage and social determinants of health, Loaiza-Bonilla said. It ranks up to 100 exact and partial matches.
“We’re able to in 17 seconds match you to all the trials available in real time,” he said. Getting this information quickly is crucial because all too often a patient might find out too late that they were a match for a particular trial that has ended enrollment.
The system can also flag potential trials the patient might qualify for down the road if their condition changes, Loaiza-Bonilla said. “We are basically putting together a list of options that you can activate in real time,” he said. “The nice thing about it is that if you are on our platform from the beginning, we can help you across your journey.”
The goal is to help more people — and importantly a more diverse group of people — participate. Increasing broad participation in research has become even more crucial in light of FDA guidance aimed at increasing diversity in clinical trials, Loaiza-Bonilla said.
Retention is crucial
However, simply getting patients into trials isn’t enough — organizations need to retain them, Del Rio said. This is where decentralized trials can excel.

Candice Del Rio, director of clinical operations, Curavit Permission granted by Candice Del Rio
Patients with cancer are already dealing with a lot and need trial options that more easily fit into their lifestyle. For instance, many patients Del Rio has worked with needed to travel from other states or even other countries to participate in a study, making the process difficult and expensive and, in some cases, requiring patients to find temporary housing. Decentralized trials can make the process easier on patients by allowing them to participate from home, requiring fewer site visits.
One reason people running clinical trials hesitate to embrace a remote option because they have less in-person contact with patients, Del Rio said. But remote trials can also offer advantages when it comes to tracking patient health in real time.
“You can get quicker notifications. Sometimes in a clinic, we wouldn’t know that someone was experiencing an adverse event for two weeks until they actually came into the clinic,” Del Rio said.
But remote monitoring allows researchers to quickly identify when something is off and respond quickly. This can also improve retention, she said, because a patient with a new symptom can get immediate help, which might otherwise lead them to abandon the trial.
When using a decentralized model, however, it’s important to incorporate some flexibility in your trial design, Del Rio said. For example, while technology can be more convenient for some trial participants, it may sometime be challenging for others. Providing options can help.
Building for the future
Overall, improving enrollment and retention in oncology trials is crucial.
“Trials are part of the treatment. In a lot of ways, it’s the gold standard because drug developers are constantly trying to find better ways to treat an illness and cause fewer side effects and prolong longevity,” Del Rio said.
While there are many reasons why patients don’t participate in trials, improving enrollment often comes down to two simple factors — improving access and communication.
“If we use [our] tool at scale and reach out to those populations, we can hopefully make studies much more accessible to those populations that otherwise may have not been able to get them,” Loaiza-Bonilla said.
Curavit partners with 1nHealth for digital first recruiting of DCT
As seen on – Outsourcing Pharma
October 18, 2022

Digital enrollment for Lark Health’s Cardiovascular Disease DCT is sped up by using the “tapestry of the entire internet” through Curavit and 1nHealth.
What’s your leadership brand?
October 14, 2022
Bringing your whole and authentic self to work is key. But what does that mean? And why is it important to have a personal leadership brand?
Experts say a brand conveys your identity and distinctiveness as a leader, communicates the value you offer, positions you as an industry thought leader and enhances your company’s brand. It can also give people a reason to follow you. As John Maxwell said: “If you think you’re leading, but no one is following, then you are only taking a walk.”
Your leadership persona should tap into your key attributes, talents and skills, but it might seem daunting to figure out what that brand should be. In a Forbes article, Devapriya Khanna, founder and CEO of 212° Brand Lab, laid out three brand builders: expression, emotional intelligence and executive presence.
First, “identify your values, vision, purpose and goals and package them into an authentic expression — so that your signature style and voice are unique, yet consistent.” Second, use self-awareness as the basis for emotional intelligence. Finally, she noted a “mindful and focused leader exudes leadership presence. Mindfulness can open the door to emotional connection with oneself and others.”
Take the time and put in the effort to create the persona that reflects your reputation as a credible and trustworthy leader who others will follow to achieve the big, hairy audacious goals for your organization.
For insights on how life science executives view their leadership style, we asked our 2022 PharmaVoice 100 honorees to identify the brands they relate most with. It’s no surprise that many pointed to top global brands — Apple, Google and Amazon — as inspiration. Interestingly, Patagonia was the No. 1 brand identified, with execs noting the company’s commitment to social responsibility, sustainability and community as values that resonate with them.
Here’s what some of the industry’s top execs had to say about their personal leadership brands.
Apple to the core
“I see Apple as a brand that is fueled by creativity, innovation and disruption. It’s a company that has pushed boundaries and been forward thinking since its beginning. I aspire to drive disruptive and innovative ideas forward, and foster the curious, creative mindset that seems to be the core of the Apple brand.”
Johnna Wesley, vice president, T1D & kidney disease research, Novo Nordisk

“Apple, because they are always striving to add value for their customers while being unrelenting in their pursuit of it.”
Jennifer Gould, director of marketing excellence, GSK

“If I were to brand myself, I would integrate the positive aspects of Google into my brand. For example, Google is widely accessible to so many people all over the world and as a champion of the decentralized model for clinical trials, one of the key benefits of that model is to make clinical trials widely accessible to all demographics. As DCTs continue to gain momentum, they will enable greater diversity and inclusion for trial participants.”
Dr. Pamela Diamond, co-founder and chief medical officer, Curavit Clinical Research

“Google, because it is colorful and doesn’t take itself too seriously but represents clear technical excellence with world changing impact
Armon Sharei, founder and CEO, SQZ Biotechnologies

“I would choose Ben & Jerry’s ice cream. There are several reasons why this is the perfect choice for me. Ben & Jerry’s has a long history of supporting and promoting social justice issues. I have tried to do the same. Ben & Jerry’s co-founders have made it their mission to protect the environment and promote sustainable food systems. Moreover, Ben & Jerry’s has supported free trade and partners with equity-related organizations. The causes Ben & Jerry’s focuses on deeply resonate with me in my life and my career. Promoting social justice in everything we do, ending systemic racism in healthcare, being a vegetarian and protecting the environment are vital to me. Finally, I love ice cream.”
Lori Abrams, former vice president, patient advocacy and clinical research diversity, WCG

“My brand would be Disney because they put customer service above all else to ensure everyone has an amazing experience. They don’t always get everything right, but they always listen to their employees, shareholders and customers and seek out their feedback for improvements.”
LaQuinta Jernigan, chief operating officer, Mdgroup

“If I were a brand, it would be The North Face. Outside of the great products they offer, the company’s mantra ‘Never Stop Exploring’ has always resonated with me. Named for the most challenging side of the mountain, the company has always encouraged its customers to push their limits, discover something new, and reach their dreams. While Karuna operates in a completely different market, we also encourage exploration, innovation and pushing the boundaries of what is possible to bring meaningful new treatments to people who need them.”
Andrew Miller, founder and chief operating officer, Karuna Therapeutics

“Patagonia: Their values are at the forefront of everything they do; their actions reflect their mission and values. With a focus on sustainability, quality, education and activism, they want to build the best products, cause no unnecessary harm, in the process and use their business to inspire and implement solutions to the environmental crisis.”
Dr. Barbara Klencke, chief medical officer, Sierra Oncology, a GSK company

Taking a Virtual Approach to Clinical Trials
As seen on – The Medicine Maker
September 29, 2022
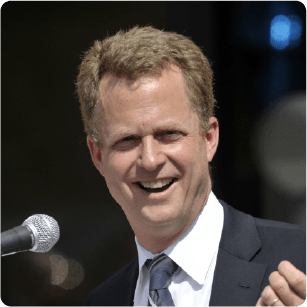
Let’s face up to facts – there are challenges when it comes to clinical trials. Patient recruitment can be challenging and dropout rates can be high. Studies often put significant pressure on patients, who must juggle personal commitments with travel and trial participation.
Working with virtual CROs, explains Joel Morse, CEO at Curavit, could be one solution to the multitude of challenges companies face. “The traditional model for clinical trials has worked well for a very long time – and it still does serve a purpose,” says Joel Morse, CEO at Curavit – a virtual CRO. “However, it is inherently complex, with multiple sites, multiple and disparate patient recruitment efforts, and multiple places where data resides. The biggest challenge remains finding patients.”
Morse is passionate about the benefits of using digital tech to improve trials. For example, digital technologies can allow patients to participate in a trial regardless of location. For example, televisits allow patients to meet with the principal investigator of the trial from anywhere via a simple web link. “Patients can report how they’re doing to trial teams via electronic diaries rather than having to go into a doctor’s office,” he says. “They can also handle the often long process of consenting to participate in a trial through e-consent applications and report on progress via e-PRO technology or electronic patient-reported outcome solutions.”
Morse also adds that technologies can enable companies to solve big challenges that are important to regulators and government, including diversity, health equity, and patient centricity. Digital technologies expand patient access to clinical trials across a wide geography because patients are no longer tied to physical trial site locations. Most trials take place at large academic institutions or academic hospitals in major cities, making it logistically difficult, if not impossible, for patients in rural or remote locations or without the financial means to take off work and travel great distances to participate. In fact, 70 percent of all clinical trials worldwide occur at just 5 percent of research sites, which primarily draw patients from populations within 40 miles of trial sites. Digital or DCT technology allows patients to participate from their own homes, eliminating the barrier of travel.
He says, “In my view, the most exciting potential of virtual trials is the ability to reach the large percentage of patients that are not historically exposed to clinical research. Virtual trials are also one of the rare instances where the regulatory environment is providing tailwinds to innovation by creating new guidelines for digital tech use in trials so they can certainly add value to trial recruitment and retention.”
But this does not mean that virtual trials are a panacea to all of the industry’s clinical trial issues. “Sometimes sponsors will try to incorporate digital technologies into a traditional trial that was not initially designed for digital. This has the unintended consequence of pushing new technology onto the trial sites without properly training them how to use it from the beginning, complicating and even slowing down the trial mid-swing,” Mose says. “If companies designed trial protocols by collaborating with DCT experts from the beginning by looking at what aspects of the trial could benefit from decentralization and building those technologies and processes in early, you have the best results.”
But Morse is optimistic about virtual trials. But believes further progress will be necessary to see their widespread use. He says, “Currently too many trials shoehorn technology into a traditional design and end up increasing, not decreasing, patient burden. One day, digital technologies and processes will be an integral part of all trials, natively designed into each one.”
ixlayer Partners With Curavit
As seen on – Applied Clinical Trials
September 6, 2022

Digital enrollment for Lark Health’s Cardiovascular Disease DCT is sped up by using the “tapestry of the entire internet” through Curavit and 1nHealth.
DE&I Champions: Dr. Pam Diamond
September 6, 2022

Editor’s note: This story is part of our 2022 PharmaVoice 100 feature.
The pharma industry is full of execs who were initially inspired to pursue a career in healthcare after seeing a doctor in action. But not many can say this interest stemmed from up-close encounters with a doctor from the von Trapp family — the family who formed a singing group together and were the inspiration behind “The Sound of Music.”
When Dr. Pam Diamond was growing up in a tiny Rhode Island town, her parents fought chronic health conditions for years while being cared for by Dr. Rupert Georg von Trapp — the oldest of the original seven Austrian von Trapp children who formed the Trapp Family Singers with their parents, Georg and Agatha.
“I was inspired to make medicine my career from witnessing Dr. von Trapp make such a difference in the lives of both my parents,” Diamond says. “He was a superb clinician.”
Diamond had her first encounter with disparities in expectations when she told her high school guidance counselor that she wanted to go to medical school, but was encouraged to pursue nursing instead. Of course, Diamond didn’t listen and not only succeeded in medical school, she soared, breaking down barriers as the only woman in her general surgery internship and then as the only woman resident during the last two years of her otolaryngology training.
After practicing medicine for almost 30 years, Diamond “decided she wanted to make a broader impact on healthcare by modernizing clinical trials,” her nominator says.
Seeing opportunities to innovate in the field, Diamond co-launched Curavit Clinical Research in 2019. The timing could not have been more challenging — and more apt. Although the pandemic brought clinical trials to a halt around the world, Curavit emerged with digital solutions just in time, becoming the first all-virtual contract research organization (VCRO). According to her nominator, there were only 617 decentralized clinical trials (DCTs) with a virtual component in 2019. In the space of just three years, that number has now swelled to 1,300 trials.
“And the benefits on clinical trial speed, access and patient diversity — even outcomes — are becoming clear,” her nominator says. “Maybe as important, the adoption of DCTs has opened a new level of innovative thinking in how clinical research gets done.”
“Undoubtedly, COVID-19 helped DCTs gain acceptance among sponsors, investigators and participants. But now stakeholders are seeing the incredible advantages of this new digital model to drive acceptance post-pandemic and beyond.”
Dr. Pam DiamondChief medical officer, co-founder, Curavit Clinical Research
To stay successful in the quickly evolving space, Diamond says she has relied on decisive thinking.
“DCTs rely heavily on technology,” she says. “If trial design decisions are not made expeditiously, the originally proposed technology solutions could become obsolete.”
DCTs have not only brought more speed and efficiency into the trial space, they’ve also been a boon for patient diversity. Diamond’s nominator notes that Black patients comprise just 5% of the research population, even though they account for 13.4% of the total population in the U.S. Yet, Diamond believes virtual DCTs may help level the research field — just one of several key advantages DCTs bring.
“DCTs provide greater access to trials, reduce trial budgets, improve population representation in trials and make rare disease research dramatically more feasible,” Diamond says.
To date, Diamond’s nominator says one of the company’s most successful efforts has been in remote digital technologies to test a hearing loss treatment developed by a Boston area biotech company.
“[Diamond] and Curavit’s Lead Audiologist, Dr. Rachel Rangel, designed a unique way to record the audiometric evaluations of patients across all sites with the recordings automatically uploaded to a cloud-based platform, accessible to the Curavit team for objective endpoint adjudication,” her nominator writes.
As an “unassuming, behind-the-scenes innovator,” Diamond’s nominator says these new approaches are being pushed forward because Diamond “replaced her white coat for a suit coat” to connect more patients to clinical trials.
Curavit, Swing team up on fibromyalgia therapeutic trial
As seen on – Outsourcing Pharma
September 6, 2022

The CRO and DTx specialist are joining forces to conduct a hybrid clinical trial of a potential digital therapeutic that is aimed at treating fibromyalgia.
For Digital Therapeutics, Virtual Trials Leverage Efficiencies
As seen on – Managed Healthcare Executive
September 2, 2022
The virtual format is catching on but has important limitations which make it unsuitable in certain situations.
The promise of prescription digital therapeutics (DTx) is the opportunity to use the ubiquitous technology to quickly and efficiently deliver therapies to patients. Increasingly, the makers of digital therapeutics are seeking to leverage those same efficiencies to streamline clinical trials.
Earlier this summer, Swing Therapeutics announced it had hired Curavit Clinical Research to be a virtual site for the pivotal trial of Swing’s investigational fibromyalgia digital therapeutics.
Under the terms of the arrangement, Curavit will recruit, screen and enroll patients into the PROSPER-FM trial, after which Curavit will manage participants over the course of the trial’s 12 weeks. The trial involves the study of 2 digital applications, which incorporate combinations of self-management skills, mindfulness activities, symptom tracking, and disease education.
oel Morse, MBA, Curavit’s chief executive and co-founder, told Managed Healthcare Executive® that digital therapeutics are a natural fit for virtual trials.
“There are no physical logistics — no shipping, storing, chain of control, cold storage, or biohazards, plus endpoints can be captured within the digital therapeutic application itself, making DCTs [digital clinical trials] ideal for studies whether seeking regulatory approval or consumer and payer confidence,” he said.
Morse said another benefit to digital trials for digital therapies is that the products by design track the most of the relevant endpoints of the trial. As a result, he said, digital therapeutics makers can avoid the need to purchase expensive third-party software to track endpoints.
That said, the virtual format is not a fit for every scenario or indication. Without a physician or other healthcare provider directly monitoring patients in clinics, certain endpoints cannot be feasibly or reliably measured in a remote setting.
Mike Rosenbluth, Ph.D., the CEO of Swing, said the fibromyalgia trial will avoid such problems because the endpoints being studied are based upon patients’ daily experiences of the disease.
“Understanding patient outcomes in their day-to-day rather than in a provider clinic is more accurate and representative of how well they are doing,” he said.
Rosenbluth said the endpoints in PROSPER-FM are all patient-reported, which is the accepted “gold standard” for fibromyalgia studies, he said.
“Even if we conducted all in-person visits, we would still collect these outcomes remotely,” said Rosenbluth.
But Rosenbluth said one benefit of the virtual design is that patients do not have to travel to receive their therapy, which is important because the condition itself can make travel uncomfortable and difficult.
“These patients can be in pain and fatigued and it is unreasonable to ask them to take on another task when getting through their day is already hard,” he said.
One of the most important facets of any critical trial is recruitment. Studies with an insufficient number of enrollees or with enrollees who do not reflect the demographics of the real-world patient population may have limited generalizability and ultimately, limited usefulness. Rosenbluth said a virtual structure can also help in this regard.
“This approach absolutely makes it easier to get a representative sample for our study population,” he said. “This has been a real challenge in previous studies in the field.”
As for the broader potential of virtual trials, Morse said it is important that any potential virtual trial be evaluated carefully for its suitability, including “taking a cautious look at things like high morbidity patient populations, complex therapies, and significant physical and/or emotional safety concerns,”
In some cases, traditional or hybrid approaches will still be most appropriate, he said.
Video: The State of Decentralized Clinical Trials | Interview
August 17, 2022
Video: How Can Pharma Improve Clinical Trials?
As seen in – The Medicine Maker
June 17, 2022
What can pharma companies do to ensure that clinical trials are conducted in the most efficient and patient-centric manner?
Clinical trials are integral to the drug development process. Yet, they are still affected by long-standing challenges, including poor recruitment and retention, the use of paper-based systems, and siloes among participating stakeholders. Though many in the industry agree that something must be done to address these challenges, practical steps are necessary to see real and lasting change.
The Medicine Maker brought together an expert panel to discuss the challenges affecting clinical and what can be done to make a difference.
Watch our video to learn more about the trends and challenges affecting clinical trials, including the growing prevalence of digital and decentralized trials, COVID-19 induced supply chain issues, and the impact the war on Ukraine is having on trials.
Participants:
Georg Schulz, EVP of Clinical Services & Senior Director of Corporate Development at Tanner Pharma Group, a global provider of pharmaceutical solutions.
Georg has more than 25 years of senior executive experience in the pharmaceutical industry. He has a proven track record in strategy design and execution, organizational development, supply chain management, international air and sea transport, and cold chain management for pharmaceutical products.
Dave Hanaman, President, Co-founder, and Chief Commercial Officer at Curavit
Dave co-launched Curavit over two years ago. He has spent more than a decade as an intelligence officer in the US Navy and was co-founder and director for 22 years of C3i, a global healthcare technology company, until it was sold.
Claire Marsden, VP, Digital and Decentralised Solutions at Medable
Claire has worked in the industry for over 25 years. She has worked across all phases of clinical development in companies including GSK, Pfizer, Novartis, Bayer Alnylam, and IQVIA.
Andrea Valente, Chef Executive Officer at ClinOne
With over 20 years of industry experience, Andrea joined ClinOne after serving as Chief Operating Officer at Medable. She has an extensive background in life sciences technology product development, delivery operations, customer loyalty, and merger and acquisition strategy.
Unique Considerations in Designing Decentralized Trials for Digital Therapeutics

Pam Diamond, MD
Digital therapeutics (DTx), the use of software-based interventions to prevent and treat disease, is one of the biggest areas of growth in life sciences. CB Insights reported that 2021 funding in the digital health industry grew 79% over 2020,{1} and the global DTx market is projected to hit $13.1 billion by 2026, up from $3.4 billion in 2021.{2} Many say digital therapeutics will re-write the future of healthcare.{3}
The DTx industry isn’t just aspirational. Studies show improved outcomes from DTx, either alone or in conjunction with conventional therapeutics, in a broad range of indications, including cancer, ADHD, asthma, schizophrenia, and insomnia. Some examples of products include video games to treat mental and behavioral health issues; a platform that incorporates neurological music therapy, sensors, and artificial intelligence to help patients who have suffered a stroke or other neurological disorder to rebuild motor skills; and a smartphone app that can conduct electrocardiograms anytime, anywhere.
Background
While exciting, this is still unchartered territory. Regulatory lines are often blurry between prescription DTx, non-prescription DTx, and combination digital therapeutics/traditional medication. It’s worth noting, however, that the U.S. Food and Drug Administration (FDA) has demonstrated its commitment to supporting digital health technologies through the publication of multiple guidance documents and the launch of the Digital Health Center of Excellence, which aims to connect and build partnerships to accelerate digital health advancements, in September 2020. In April 2021, too, the FDA loosened regulations surrounding approval of digital mental health tools to hasten their time to market.{4}
Even so, not all DTx manufacturers choose to seek FDA approval, but they all need to prove efficacy through clinical studies for payers to consider coverage and consumers to consider purchase. Regulatory approval is not always the end goal—or at least, not initially.
AstraZeneca, for instance, has designed a rigorous and low-patient-burden digital therapeutic to monitor metastatic breast cancer patients. The prescription DTx, which is currently being tested in clinical trials in 23 countries, was developed using insight from a review of medical literature, pulmonary and breast cancer experts, technology review, and real-world evidence gathered through conducting a deep cohort analysis of approximately 500 patients in U.S. health systems.{5} The therapeutic’s aim is to monitor patients’ symptoms and vital signs and, based on algorithms and expert rules, alert a physician as to how well the patient is doing on the treatment to maximize both safety and outcomes.
“Regulation will differentiate between a fitness app a consumer can simply download, with no regulation required, versus something that is scientifically proven to have a direct impact on someone’s health condition or outcome, which a doctor may prescribe,” said Cristina Duran, chief digital health officer for AstraZeneca, in a statement. “In a few years, I think we will see that shift to it being commonplace for your doctor to prescribe a digital therapeutic, a medication, or both.”
Indeed, it’s a complicated and quickly evolving arena in healthcare.
On top of the current regulatory limbo, DTx manufacturers face many of the same clinical trial challenges as traditional drug makers, including those tied to patient recruitment and retention, quality of data, and costs. They also must carefully consider the unique technical security concerns of an all-digital therapeutic and face strategic decisions around either provisioning smart devices or leveraging a “bring your own device” (BYOD) policy. At the same time, clinical trial models are rapidly evolving, adding further complexity for companies working to develop innovative digital therapeutics in a post-pandemic environment. Decentralized clinical trials (DCTs) are becoming a preferred model for research in biopharma and offer even greater benefits to companies conducting studies on digital therapeutics.
Wave Neuroscience, a medical device manufacturing company that specializes in designing software and physics-based personalized brain-based interventions, is moving toward more decentralized clinical trial designs. “DCTs can improve patient recruitment and retention by reducing burden and eliminating geographic barriers,” explained Dr. Erik Won, president and chief medical officer of Wave. “This also results in a more representative sampling of the population, such as patients from rural areas who often don’t have access to major institutions.”
Dr. Won continued, “DCTs can also increase the quality of data by minimizing the Hawthorne Effect—where individuals modify an aspect of their behavior in response to their awareness of being observed, also known as ‘white coat syndrome’—because patients are in their home environment.” Finally, DCTs can be more cost-effective, he added.
When Stars Align: DCTs and DTx
Fundamentally, a DTx is software rather than a pill or injectable, so there is no distribution or administration of medicines. There are no physical logistics—no shipping, storing, chain of control, cold storage, or biohazards—plus endpoints can be captured within the DTx application itself, making DCTs ideally suited for DTx studies whether the goal is regulatory approval or consumer and payer confidence.
In all cases, though, the unique advantage is that the DTx being studied in a trial is also the data collection device, so manufacturers often don’t need extra technologies like an electronic patient-reported outcome (ePRO) system to capture data in a clinical trial. It’s all in one, and this can result in big cost savings.
For example, Texas A&M and Wave Neurosciences are conducting a hybrid clinical trial on the safety and efficacy of magnetic EEG-guided resonance therapy to treat post-traumatic stress disorder (PTSD). This therapy uses transcranial magnetic stimulation, which has been cleared by the FDA for treatment-resistant major depressive disorder, obsessive compulsive disorder, and nicotine cessation. With this algorithm-driven therapeutic, a personalized treatment is delivered via conventional (in-person) appointments. Screening and follow-up visits, in which participant-reported data are collected, take place virtually to the extent possible.
“America is experiencing a crisis in mental health,” said Dr. Won. “Software- and physics-based personalized therapeutics are a modern, non-pharmaceutical, non-invasive option to help in this area. We are testing our therapeutic with an eye to pursuing an FDA marketing approval for the PTSD indication. We are exploring the decentralized trial model to introduce greater flexibility and speed into our research efforts.”
Best Practices for Designing DTx Trials
With the quickly growing and evolving DTx market, and the complexities associated with clinical research, here are five considerations for decentralized trial design:
- Know your regulatory roadmap before embarking on a trial.
Because the regulatory pathway for digital therapeutics is not as clear-cut as it is for traditional investigational drugs, it is critical to outline your regulatory roadmap before recruiting the first patient. Feasibility studies can be a good place to start, especially to help map out an expansion plan down the line. Some important considerations also include how future versions of your DTx product will be tested, benchmarked, and evolve over time.
“It is always best to seek meetings with the FDA’s device division [the Center for Devices and Radiological Health] early, and often,” said Dr. Daniel Karlin, chief medical officer at MindMed, a clinical stage biopharmaceutical company developing novel products to treat brain health disorders. Dr. Karlin is also the lead medical advisor to the makers of the first and only FDA-cleared, prescription DTx that improves sleep in adults 22 and older with nightmare disorder or nightmares related to PTSD.
Dr. Karlin continued, “It is easier for DTx providers to secure meetings with the FDA because digital therapeutics are typically less biologically complex and therefore pose less risk. Request a meeting at the start of your development efforts to agree on the claims you plan to make based on the indication for use, and to establish what related evidence will satisfy the FDA. This is fundamental. Also, seek institutional review board [IRB] clearance on anything that could conceivably be research-related before you bring an experimental device to humans for studies.”
Of course, regulatory approval—while often considered the ultimate validation for the safety and efficacy of a drug or device—isn’t the only reason for conducting clinical research, especially with DTx. Health economic outcomes and human factor research are often equally important for product adoption. Even in the digital realm, real-world function and outcomes are important to create products that lead to meaningful outcomes for patients. “All manufacturers want payers and patients to be confident in our product’s efficacy, safety, and economics,” added Dr. Won.
For instance, some DTx products that have minimal risk may not require regulatory approval but are just as valuable as those that do. Decide if regulatory approval is on your short-term or long-term roadmap and design the trial accordingly. If it is not, then there is greater flexibility in study design.
- Map out an immediate and long-term commercial strategy.
Given how quickly the DTx marketplace is evolving, the best that can be done may be to sketch out a preliminary commercialization strategy that has plenty of leeway to deviate from that path, if necessary. For instance, if your therapeutic will not be intended for regulatory approval, you may need to focus on a consumer strategy that focuses on everyday wellness. If you know this up front, you can design your clinical trial around endpoints that mirror your target consumer’s biggest pain points. However, if your end-goal is to develop a DTx that will be used in combination with an FDA-approved drug, then you will need to design your trial based on endpoints relevant to that drug maker’s target patient population.
- Carefully consider and incorporate protections against technical security breaches.
Data security and privacy are crucial for all clinical trials, but especially when studying DTx that are 100% tech-driven and, therefore, potentially vulnerable to more issues. One of the most important decisions that needs to be made up front is whether the protocol will strictly enforce a BYOD strategy (which could prevent some patients from participating) or require the sponsor to provision devices to all participants (which could be cost-prohibitive)—or some combination thereof. Each option comes with different security considerations, so decide this up front.
Regardless of device strategy, all data collected on the smartphone will need to be encrypted and then sent to a secure central platform in the cloud that follows all regulatory compliance parameters. Additionally, invest in a platform provider or tech-enabled CRO that maintains a strict security perimeter, including a “zero-trust” architecture with individual logins and audit trails for everyone who has access to the data every time they log in or out—this, on top of the digital therapeutic app’s security standards.
- Develop digital endpoints that are fully validated and meaningful to patients.
Traditional medicine trials measure against accepted endpoints that are validated in accordance with standards set forth by the IRB and regulatory organizations. However, DTx studies are typically measuring novel digital endpoints that are different for each DTx app and do not have a history of vetted benchmarks against which to be validated. Even so, reviewers will need to ensure that the novel endpoints aren’t bogus, and this can require some extra steps and creativity.
In many cases, endpoint validation in DTx studies requires a comparison to something similar that has been already validated or the use of previously vetted ratings scales. For example, when conducting a depression study, the DTx sponsor may first administer the Columbia-Suicide Severity Rating Scale—a suicidal ideation and behavior rating scale created by researchers at Columbia University, University of Pennsylvania, University of Pittsburgh, and New York University—to potential participants at screening. The patient’s score can be the baseline for the study, so if the DTx is efficacious, that score should drop and serve as a validated digital endpoint for symptoms of depression.
Similarly, DTx studies may leverage ePROs to administer quality-of-life questionnaires compared against prior research already accepted and validated by the IRB and FDA. Another way to validate endpoints in a decentralized DTx trial is to incorporate an initial site visit with a clinician who can compare the measurement of, say, a wearable device against an equivalent onsite, hospital-grade machine. Doing so can prove the wearable is as valid a measuring tool as another.
Finally, as important as endpoint validation is patient validation—in other words, identify the measurements or endpoints that are meaningful to patients. For example, with Fern Health’s digital musculoskeletal platform, the company shifted the focus of pain management from pain relief to functional restoration. Early on, the company found that functional pain endpoints are more important to patients in the long term than pain relief alone and made that critical adjustment.
- Assess the use of DTx placebos or sham apps early and often.
In a DTx clinical trial, dummy or “sham” apps are often used as a control in comparison to the actual treatment or intervention app—like a placebo pill used in a randomized control trial. There are unique considerations in using sham apps, however, including the potential for an unintentional placebo effect.
Here is the challenge: It is very difficult to make a sham app similar enough to the real one, which means patients often suspect that they were not assigned to the treatment arm. In addition, patients who do interact with the sham app can experience a placebo effect that negatively skews study results. For instance, patients in the treatment arm of a study would typically show significant symptom improvement compared to the non-treatment arm, but when using a sham app, that disparity is not as dramatic.
The FDA has not yet ruled on whether placebos or “sham” apps must be used in DTx trials, but the agency often prefers a sham control. DTx companies that opt not to use a sham control will need to work very hard to find creative ways to design an FDA-acceptable trial that won’t be criticized—even then, there is no guarantee that the FDA will accept the results.
“It is highly unusual to view sham controls as unnecessary in clinical trials,” said Dr. Karlin. “Not only do regulatory bodies prefer sham-controlled evidence in digital therapeutics studies, but also clinicians. Reluctance to use sham apps will cause companies to struggle to get both FDA clearance and physician buy-in, which is critical for commercial success with patients.”
Dr. Karlin’s team for the PTSD DTx leveraged a sham control on a wearable device that, rather than buzz when detecting a nightmare, simply recorded it. “When we assessed the reliability of our blind through a survey of our trial participants, we found that most did not know whether they were using the real therapeutic or the sham,” he noted. “This helped validate the research because it meant that we could reliably compare the active intervention with the placebo for more meaningful results. Randomization and sham control are not magic bullets, but they’re the best options we have right now.”
As the Digital World Turns…
There’s still a lot to be learned in the DTx market, but they are here to stay with growing reliance, trust, and adoption of digital health products. COVID-19 pushed researchers to lean into the decentralized model for research, and the pandemic has simultaneously fueled a growing need for DTx products—an ideal marriage of process and product. Remaining flexible and open-minded will be critical to succeed in this evolving and exciting area—as the digital world turns.
References
- Taylor NP. 2022. Digital Health Funding Jumps to New High. MedTech Dive. See full resource here.
- Market and Markets report. 2021. Global Digital Therapeutics Market Projected to Reach USD $13.1 Billion by 2026. ReportLinker. See full resource here.
- Taranto B. 2021. The Growing Power of Digital Healthcare. TechCrunch. See full resource here.
- Staff report. 2021. DTx Trends and Companies to Watch in the Growing Digital Health Industry. Insider Intelligence. See full resource here.
- Galbraith S. 2021. Digital Therapeutics: Augmenting Patient Outcomes. AstraZeneca. See full resource here.
Digital Therapeutics Deliver Surprising New Benefits for Cancer Patients
June 7, 2022
Digital technologies have had profound effects on how we communicate (i.e., smartphones), share information (i.e., social media), and create (i.e., 2- and 3-D printing). Now, they are having an impact in healthcare, too. The latest (and arguably most exciting) example is digital therapeutics (DTx): medical treatments to address health conditions via a combination of software and communications. DTx are in use or being tested for a growing list of diseases and conditions: Type 2 diabetes, congestive heart failure, obesity, Alzheimer’s disease, dementia, asthma, substance abuse, hypertension, anxiety, depression, and more.
Digital Health or Digital Therapeutics?
Researchers and policymakers make distinctions among digital health (the overall category of health-related interactions), prescription digital therapeutics (apps or tools that have gained regulatory approval), and software used as an adjunct to guide a healthcare provider’s treatment of a patient (software as a medical device, or SaMD, regulated in the US by the FDA Center for Devices and Radiological Health). There are overlaps from one category to another but, in nearly all cases, a rigorous evaluation in the form of a clinical trial to clearly demonstrate the impact of the digital technology is needed, even when regulatory approval is not the end goal.
“Digital solutions have a variety of intended use cases which drive their approval pathway, and they are equally valuable and important depending on the end goal,” said the head of digital health, oncology R&D at a top-10 pharmaceutical company that has digital therapeutics in development across therapeutic areas. “Whether the digital therapeutic is for consumer health assessment or in a trial or routine care setting, following the guidance around use cases and a carefully developed measurement framework is critical to ensure scientifically rigorous and responsible assessment of a patient’s health status.”
In parallel with the maturation of DTx, numerous researchers have been examining the social or patient-centered aspects of oncology care, especially now that oncology care is becoming a participant in the DTx evolution. The opportunities for improving health outcomes in oncology through DTx arise from challenges expressed by many cancer patients: surgery, radiation, chemotherapy, and/or immuno-oncology, all carried out over several years and with substantial side effects. Sleep, eating patterns, and physical activity can be affected. For many patients, simply withstanding the course of treatment is a victory, let alone what happens to their cancer.
Researchers think that digital therapeutics can help. One pre-market prescription DTx company dedicated to improving mental health in cancer patients is conducting various clinical trials on new DTx products designed to improve cancer-related distress that affects a patient’s quality of life or ability to cope with cancer diagnosis and treatment, which affects nearly half of cancer patients. According to the company, “digital therapeutics that help to treat cancer-related distress have the potential to help close the cancer treatment gap.” DTx products may incorporate cognitive behavioral stress management, which has been tailored to cancer patients and shown in numerous clinical studies to improve emotional well-being, physical health, and overall survival.
“We will continue to prioritize the study and development of digital therapeutics for real-time, continuous patient monitoring, from side effects of treatment to symptoms of disease that indicate progression. The aim is to allow patients to stay on therapy longer, have fewer side effects and adverse events, wherein this improved treatment tolerability may potentially lead to increased benefit from therapy,” added one top-10 pharmaceutical company’s head of digital health.
For at least the past decade, researchers have been documenting longer survivals, better adherence to therapy, and improved quality of life (QoL) when various forms of digitized health or therapeutic actions are taken. A lung cancer study comparing symptom monitoring using a DTx versus the standard process conducted in France in 2017 was so successful that it was prematurely halted and patients in the control group were transferred to the study group receiving the digital intervention. The median overall survival was 22.5 months in the digital intervention group versus 14.9 months in the control group.
Another app-based symptom reporting study at Memorial Sloan Kettering found a five-month extension of median overall survival among solid-tumor cancer patients, along with improvements in QoL during treatment. “One potential mechanism of action is early responsiveness to patient symptoms preventing adverse downstream consequences,” the researchers summarized.
Despite these early successes, organizations often must run clinical trials to reinforce the value of digital intervention to all stakeholders including not just regulators, doctors, and patients but also payers, who seek health economics data. DTx manufacturers are increasingly leaning into the decentralized clinical trial (DCT) model for its speed, efficiency, data quality, and patient-centric advantages.
Now a widely accepted trial model in the aftermath of the COVID-19 pandemic, DCTs use software to connect patients to trials. Travel to and from the trial site is minimized or eliminated; interaction with trial participants can be frequent (or, in cases where wearable medical devices are involved, it can be 24/7); and there are few geographic limitations, so participation can be more representative of the population.
In addition, there is a fundamental alignment between a DTx and a DCT. Since DTx is software rather than an oral or injectable formulation, there is no physical distribution or administering of medicines, just as there are often no physical sites in a DCT. There are no logistics: No shipping, storing, chain of control, cold storage, or biohazards; in addition, endpoints can be captured within the DTx application itself, making DCTs ideally suited for DTx studies. In the case of combination DTx/traditional studies in oncology, however, there will likely need to be some in-person site visits, so a “hybrid DCT” approach may be ideal.
Here are three key benefits of hybrid DCTs in oncology DTx development:
DCTs Boost Patient Recruitment, Retention, and Engagement
Decentralization Improves Cost Efficiency
DCTs save costs, in part, by saving time. For instance, the single biggest time drain in drug clinical trials is patient recruitment, which can take about one-third or more of the duration of the entire trial and contributes to a trial’s high price tag. Similarly, recruiting a diverse patient population and keeping them engaged for DTx studies is draining. By expanding the geographic area for recruitment, DCTs speed recruitment across a more representative patient population. By removing many of the burdens associated with traditional trials, DCTs decrease dropout rates in DTx studies.
In addition to the financial benefit that comes from saving time, DCTs require less staffing and greatly reduce the need for sites and infrastructure. In fact, for many growing DTx companies, lengthy brick-and-mortar trials are unnecessary because they don’t have the same scope or needs as a randomized phase 2 or phase 3 study. The technology that DTx companies need to run a trial is materially different from the technology needed for a traditional drug trial. Further, much of the software needed for a DTx trial is already baked into the DTx app used in the study, so many of the components (such as EDC software) required for traditional clinical trials involving prescription drugs are not needed. This is not to suggest that a decentralized clinical trial is any less valid–just more innately streamlined. As a result, DTx companies can save substantially–reducing the costs by a factor of 20 or more–by picking just the technology needed rather than paying for complete functionality of an application or irrelevant bells and whistles.
This benefits the patient, too. Patients who use one app to complete all trial forms find participation much easier than using different devices or going into a site for repeat visits. Again, a better patient experience decreases study dropout rates and results in even greater savings and improved trial data.
Data Quality Improves with DCTs
“Digital therapeutics are prescribed by a doctor often alongside a medicine, so it’s very reasonable to expect that we’ll see more DTx and drug combination regimens emerge in oncology in coming years,” concluded one top-10 pharmaceutical company’s digital health leader. “Combining innovative new treatments with evidence-based digital health solutions is one way we can think more holistically about cancer patient care to improve health outcomes.”
Invest in Technology, Profit in Better Health Outcomes
June 7, 2022
Improving preventative care and chronic disease management has helped slow the process of aging. In the United States, the 65 and older population has grown by over a third in the past decade, and the number of adults aged 85 and older is expected to nearly triple by 2060. Yet, living longer comes with risk. Genetic mutations are generally managed by the body’s ability to perform necessary repairs. However, with increasing age, the number of mutations also increases, which can give rise to cancer. Indeed, people aged 67 and older represent half of cancer patients and cancer is the second leading cause of death for people aged 85 and older. We owe it to ourselves to do something about this.
While the primary purpose of research is to learn, clinical research also seeks to advance treatments if possible. Many oncology patients, particularly those with aggressive disease, know that access to the most advanced medicines may entail being a part of a clinical trial. In comparison to other disease groups, cancer trials have the fewest age caps for enrollment. This is partly because, unlike chronological age or the number of years alive, physiological age (or how old one is due to genetics and lifestyle) is a better indicator of a patient’s ability to tolerate harsh treatment regimens and related toxicities. Older age is generally associated with reduced organ function and poorer performance status scores, which are risky for institutions ill-equipped to manage therapy-induced complications. Furthermore, sponsors would prefer to minimize instances of negative effects from their drugs; in response, many cancer clinical trials have an upper age limit of 70 to 80. Disappointingly, the median age of cancer participants enrolled in trials is an average of 6.49 years younger than that of patients with the same cancers not enrolled in trials. In essence, cancer patients who are granted entry to clinical trials are typically younger, fitter, and likelier to tolerate research regimens, while older, higher-risk patients are left without immediate access to potentially life-prolonging therapy. The very people who are most likely to require treatment with innovative therapies will not reap the benefits of a rigorous testing process.
Fortunately, these same patients are widely adopting technology: More than half of US adults age 65 and older own smartphones and 75% use the internet. Cancer patients are more likely to complete web-based questionnaires than paper-based forms. Oncology researchers often consider in-person follow-up essential to ensure safety and wellness in study participants. But this begs the question of whether the risk of missing an in-person observation outweighs the risk of transporting the infirm. Unless patients are so sick as to require hospitalization, are they not better off in the comfort of their homes, avoiding communicable infections for at least part of a trial’s duration?
One study shows that cancer patients who are offered the telehealth option improved communication with their providers, had 38% fewer hospital admissions and 31% fewer readmissions, and improved quality of life. This is significant because older cancer patients prefer quality of life over length of life. For cancer patients, untreated symptoms like gastrointestinal upset and pain can turn serious rapidly. Digital in-home symptom tracking tools for patients receiving chemotherapy offer pattern-recognition, severity detection, and real-time symptom management which reduce symptom burden by 43%, decrease the number of emergency room visits, and mitigate costs.
Advances in technology allow us to play 4-D video games, turn down our home’s heat while traveling in another state, and print objects from a personal-use device, yet we go about clinical research in an archaic fashion. Investment in our health is surely as important as investment in fun-to-haves, and yet trial participants remain too familiar with paper surveys, long clinic visits, and delayed responses to adverse events. If there is ever a time for clinical research to get up to speed with technology-driven industries, it’s now. And elderly cancer patients must be the focal point of this endeavor.
There are already pioneers committed to this mission. The Collaborations in Health, Aging, Research, and Technology (CHART) at the University of Illinois at Urbana-Champaign has constructed a research-focused “smart home” to learn how the elderly may benefit from using smart appliances, assistive robotics, and home sensors. Tools like these may seem like a luxury to some but could be essential for those who would otherwise rely on caregivers to meet basic health needs and achieve a sense of normalcy. If access to these tools improves someone’s ability to participate in a clinical trial–because they can now do just about anything a younger, healthier person can do, just differently–industry sponsors should pay attention. One cannot discount the cost of owning smart devices and tools. Insurance coverage and reimbursement programs could make a big difference in affordability. Traditional (less new) technology often carries the benefit of reduced or no cost for use. Examples include phone applications, wearable devices, and voice-operated mobile assistants.
It is important to note that some barriers to maximizing technology use in the elderly do exist. For instance, difficulty reading from small screens, manipulating voice-activated software, and understanding evolving terminology are a few. But these challenges are not insurmountable. Understanding how the elderly utilize technology is a step in the right direction. By engaging multidisciplinary research teams in rich discussions with patients and their caregivers, the potential for developing truly smart, customizable technology is vast. It may not be long before augmented reality glasses can be used for easily viewing and completing drug diaries as well as participating in virtual health visits. An automated call to a clinician when an in-dwelling catheter detects low levels of circulating red blood cells may be just around the corner. A bit of foresight, some creativity, and an incorporation of technology can allow investigators to spend more energy focusing on collecting and generating meaningful remote follow-up data that eventually improves treatment access and outcomes for elderly patients.
At present, we can only hope that our parents, grandparents, and even our future selves, if faced with cancer, will thrive in old age–not alone, but with the companionship of our aging loved ones. We can make this a reality by applying technology and thinking “outside of the (clinic) box” to bring our cancer clinical research to our elderly cancer patients.
Decentralized Trials Begin to Show Their Value in New Ways
The more experience clinical research professionals gain in conducting full or hybrid (onsite/offsite) decentralized clinical trials (DCTs), the more advantages beyond simple economics and convenience for patients they are realizing from the tactic, contributors to the next issue of ACRP’s Clinical Researcher journal suggest.
For example, in her forthcoming column on “Unique Considerations in Designing Decentralized Trials for Digital Therapeutics,” Pam Diamond, MD, cofounder and chief medical officer of Curavit Clinical Research, quotes an expert from the medical device arena as saying that DCTs can increase the quality of data by minimizing the Hawthorne Effect—where individuals modify an aspect of their behavior in response to their awareness of being observed. This phenomenon, also known as “white coat syndrome” in healthcare situations, is thought to be less of a factor when patients are in their home environment.
Diamond goes on to write that, “Fundamentally, a digital therapeutic (DTx) is software rather than a pill or injectable, so there is no distribution or administration of medicines. There are no physical logistics—no shipping, storing, chain of control, cold storage, or biohazards—plus endpoints can be captured within the DTx application itself, making DCTs ideally suited for DTx studies, whether the manufacturer’s goal is gaining regulatory approval or consumer and payer confidence.”
Meanwhile, in a column on “The Ecosystem of Decentralized Clinical Trials: It Takes a Village to Modernize Care,” MaryAnne Rizk, PhD, chief strategy officer for Medable, notes that, when “companies coordinate their efforts to design and execute DCTs, sponsors, investigators, and patients see the benefits. A connected ecosystem of DCT collaborators can streamline operations and data collection and resolve interoperability challenges. With a coordinated approach, the industry will accelerate this new model to make better medicines faster, safer, and more effective for every biology around the world.”
Rizk adds that, to navigate the new waters of DCT delivery, leading organizations are coming together to create a network of “best-of-breed, trial-enablement providers” that “includes contract research organizations, traditional and nontraditional investigator sites—including new retail pharmacy sites—and leading data and technology services providers” responsible for a range of trial support technologies and processes.
Still, Kristin Mauri, solutions services director for Remarque Systems, in her column on “DCTs: Key Considerations for Small-to-Midsized Biotech and Biopharma Companies,” looks at how the DCT trend may seem daunting for companies that feel that “the risks of treading this new territory—an area with complex data management demands and no clear regulatory guidance—outweigh the potential rewards.” However, Mauri adds that if some companies feel that DCTs are outside their comfort zone and budgets, that is not necessarily true.
As just one consideration, Mauri notes how, “untethered from sites, DCTs can recruit from anywhere, which often leads to faster enrollment and fewer screening failures. Further, that same geographic freedom also means fewer sites, thus fewer review boards, potentially lower regulatory costs, and greater flexibility around protocol amendments.”
Further, in his column on “A Hybrid Approach to Decentralized Clinical Trials,” Clincierge Cofounder and CEO Scott Gray writes that, “Moving forward, we must continue to assess the value provided by DCTs in ensuring patient experience and safety remain of the utmost priority. We should continue to build upon what has been learned since the onset of the pandemic. It is up to clinical trial stakeholders to determine the best approach for balancing the needs of patients and their caregivers against the goal of contract research organizations and pharmaceutical study sponsors. Whether that means a decentralized, traditional, or hybrid course, prioritizing clinical trial patients’ health and best interests ultimately encourages higher enrollment, increased retention, and more robust data collection results.”
The June 2022 issue of Clinical Researcher, with these columns and other content touching on DCTs and data analysis for trials, in addition to three peer-reviewed articles, will go online on or around June 21 on the ACRP website.
DCTs are also the focus of a recent whitepaper on Decentralized Clinical Trials: Perspectives for Clinical Research Professionals developed by expert members of the ACRP Fellows and sessions presented at April’s ACRP 2022 conference (such as by thought leaders from Clario and Northwell Health), the recorded contents of which will soon be available in the Online Conference Library.
Digital Therapeutics Companies Lean into Decentralized Clinical Trials
March 25, 2022

While digital therapeutics (DTx) companies are extremely optimistic about the promise of software-based interventions to prevent and treat diseases, they are still navigating unchartered territories around the best practices for clinical research, including patient recruitment and retention, quality of data, high costs, and uncertainty around regulatory guidelines.
At the same time, clinical trial models are rapidly evolving, adding further complexities. But one thing DTx companies do agree on is that the decentralized clinical trial (DCT) model is key to overcoming their biggest hurdles and improving the entire clinical research process.
A Patient-Centric Approach
Patient retention and engagement have long been challenges in clinical research, but DCTs have had a uniquely positive impact on DTx studies. DCTs make trials more accessible to participants who live far away from study centers. Opening studies up to more participants, optimizes the patient pool and reduces the need to over-enroll based on anticipated attrition or drop-out to improve cost efficiency.
Dr. Mike Aratow, Co-founder and Chief Medical Officer of Ellipsis Health, a DTx company that developed the first voice vital sign to quantify and manage depression and anxiety, explains, “A decentralized model not only aids patient recruitment because it removes many of the burdens associated with traditional trials, but it also makes it easier to reach underrepresented groups and those from a wider geographic landscape, providing real-world evidence and ecological validity. In traditional research, a significant amount of the medical data can’t be reproduced due to issues around patient retention and patient participation.”
Feel Therapeutics develops digital biomarkers and therapeutics for mental health using a proprietary wrist-worn wearable device. It monitors various physiological signals to extract insights on patients’ psychological and physical health. According to Feel CEO George Eleftheriou, “DCTs help optimize patient recruitment and improve engagement and retention. Wearable and digital technologies remotely measure endpoints while engaging participants in an unprecedented way and which naturally aligns with digital therapeutics that are intended to integrate into patients’ everyday lives. It is indicative that participants in our digital programs use our app for over 55 minutes per week.”
Reduced Costs
In 2020, Insider Intelligence predicted the global DTx market would hit $9 billion by 2025, but a year later sharply upped that forecast to $56 billion.1 Despite this market growth, the DTx industry is still in its infancy with most companies considered startups with modest resources. Cost efficiency is central to their success—and another reason why a DCT model complements the DTx business strategy.
DCTs save costs, in part, by saving time. For instance, the single biggest time drain in clinical trials is patient recruitment, which can take up to 30% to 40% of the duration of the entire trial process. By streamlining this process using digital tools and expanding the geographic area for recruitment, DCTs have faster recruitment, and require less staffing and infrastructure. DCTs allow researchers to customize DTx trials based on exact needs, patients, and commercialization strategy.
Additionally, the technology needed to run a DTx trial is materially different from the technology for traditional trials. Much of the software needed for a DTx trial is already baked into the DTx app being studied, so many of the robust components required for traditional clinical trials involving prescription drugs are not needed. DTx companies can save substantially—reducing the costs by a factor of 20 or more—by cherry-picking just the technology needed to run the DCT.
New data backs up the value of DCTs. According to a 2022 study by the Tufts Center for the Study of Drug Development, which compared published benchmarks on trial cycle times and costs with data from more than 150 DCTs conducted by trial software firm Medable, decentralized Phase 2 studies are completed one to three months faster than traditional trials and the time savings yield a net benefit that is up to five times greater than the upfront investment required. Decentralized Phase 3 trials with similar time savings yielded a net benefit that is up to 14 times greater the upfront investment.2
Improved Data Quality
Decentralized trials enable DTx companies to collect real-world data direct from patients where they are most comfortable, which has a quantifiable impact on data quality.
Dr. Erik Won, President and Chief Medical Officer of Wave Neuroscience, a DTx company that specializes in treating brain disorders, explained, “DCTs increase the quality of data by minimizing the Hawthorne Effect—a reactivity in which individuals modify an aspect of their behavior in response to their awareness of being observed, also known as ‘white coat syndrome’—because patients are in their home environment. With a decentralized trial, we get the best of both worlds. We can use other mechanisms to ensure that patients are following protocols while ensuring compliance. For instance, we record EEGs using wearables and ask patients to complete simple online surveys.”
DCTs also enable researchers to capture data and endpoints directly within the digital therapeutic itself for seamless data capture and less potential for “lost” information.
“DCTs enable us to collect passive, continuous, and objective data from users 24/7/365 and move from episodic patient-reported outcomes to continuous data collection,” added Feel’s Eleftheriou. “This rich data provides real-world evidence and allows us to explore novel biomarkers or digital endpoints in neuroscience and other chronic conditions with a high prevalence of mental health comorbidities, such as multiple sclerosis, certain cancers, and cardiac problems.”
Regulatory Approval
DTx companies operate in a nebulous regulatory environment, even as the Food and Drug Administration (FDA) works to clarify requirements. For example, the FDA has demonstrated its commitment to supporting digital health technologies recently through the publication of multiple relevant guidance documents as well as the founding of the Digital Health Center of Excellence (DHCoE) in the fall of 2020.
Yet, the regulatory landscape is complex, evolving quickly and differently in each country. Regulatory approval is not always required to go to market, disincentivizing studies. Many DTx manufacturers are left to make decisions on their own on whether they choose to seek regulatory approval, depending on their commercialization strategy and often take a bifurcated approach—seeking FDA approval for one variation of their product and not for another.
Wave Neurosciences follows FDA guidelines for conventional trials while making adaptations in non-FDA studies to maintain regulatory compliance. These “bridge” studies are often smaller, faster, less expensive and designed to gather enough validated data to determine if taking the next step to an FDA-approval study makes sense. In these cases, especially, a decentralized model makes it much easier and faster to stand up a “bridge” trial for DTx companies looking to determine what the next best steps should be for their product and commercialization strategy.
The Perfect Pairing
Fundamentally, DTx products are software, so there are no physical logistics—no shipping, storing, chain of control, cold storage, or biohazards plus endpoints can be captured directly within the DTx application, making DTx studies ideally suited for the digitally enabled decentralized model.
Even so, much is still to be learned in the emerging DTx market. While COVID may have forced researchers to lean into DCTs and the pandemic continues fueling a growing need for digital therapeutics, this perfect pairing will only benefit the industry and society a whole.
References:
1. Insider Intelligence, “DTx Trends and Companies to Watch in the Growing Digital Health Industry,” by Staff (July 29, 2021). See full resource here.
2. FierceBiotech, “Not Just for a Pandemic: DCTs Pay Off Financially, a Study Shows,” by Gareth Macdonald (January 12, 2022). See full resource here.
Despite rapid DCT evolution, there’s still room for progress: Curavit
As seen in – Outsourcing Pharma
March 9, 2022

A leader from the VCRO shares how far the industry has come with decentralized adoption, where opportunities for improvement exist, and what lies ahead.
While the pandemic knocked many clinical trial operations for a loop, the decentralized clinical trial (DCT) format has fueled a comeback since COVID-19’s arrival. Dave Hanaman (co-founder, president, and chief commercial officer of Curavit) spoke with Outsourcing-Pharma about progress made, lessons learned, and the road ahead.
OSP: How have decentralized trials evolved in the past two years?
DH: The biggest evolution has been the adoption of decentralized clinical trials (DCTs) by sponsors that would not have considered them without the catalyst of the pandemic. Before the pandemic, DCTs accounted for only 2-4% of trials and were projected to increase about 10% over the next 10 years. The pandemic and lockdowns forced the industry to get creative.
While there was a feeling early on that the use of DCTs might decline when the pandemic was over, the benefits of the model and the continued threats of new COVID variants proved otherwise. Now the DCT market’s estimated value is a staggering $1.63b USD by 2027, an annual growth rate of 14.8%, according to Precision Reports.
Much of this growth over the past six to 12 months is a result of the exploding digital therapeutics (DTx) market and their adoption of DCTs. According to Report Linker, the global DTx market is projected to reach $13.1b USD by 2026, up from $3.4b USD in 2021. These DTx companies are bringing novel software-based therapies and diagnostics into the market and their business and delivery models line up almost perfectly with DCTs because of the way these trials are designed from digital-first principles.
Gaining real-world results from a decentralized trial
February 8, 2022

When Lark Health decided to embark on its most recent decentralized trial with Curavit, a virtual CRO, its leaders saw the potential for a host of benefits.
According to OraLee Branch, the trial’s principal investigator and Lark’s director of clinical studies and research, a decentralized clinical trial (DCT) would be more patient-centric and convenient. It could boost efficiency, would likely be faster, and could help with recruiting a diverse population.
Lark joins an increasing amount of small to midsize companies now transitioning to DCTs, which provide solutions for a number of common logistical headaches.
It was also a natural fit for the midsize digital therapeutic company, which uses a cognitive behavioral therapy approach to create mobile apps aimed at managing and preventing chronic diseases, such as diabetes and hypertension. The apps’ features also include personalized coaching, and use artificial intelligence to help support lifestyle changes, such as weight loss, quitting smoking, or managing stress.
“I came to Lark from an academic background. I was a principal investigator and a full professor at various leading medical universities. So, I have a lot of experience in clinical trials and in managing decentralized, multi-site institutional trials,” Branch says.
For their upcoming study, which will test the use of a chronic disease prevention and management program, Lark wanted to enlist the help of other experts.
“We wanted a CRO who has had this kind of expertise, so that we can focus on what Lark does best, which is have great programs and great experiences for the user,” says Branch.
As an added bonus, they hope that having an outside CRO coordinating and managing data will bolster data integrity.
“We want this to be a high data integrity representation and the easiest way to do it is to have that external collection,” she says.
Here, Branch discusses how Lark plans to gain from using a DCT and how it is overcoming challenges associated with this approach.
PharmaVoice: What advantages do you hope decentralization will bring in terms of recruitment?
OraLee Branch: In conventional trials, which are typically brick and mortar or in-person trials, the people who end up participating are a select group. They are what you’d call a biased collection of participants. These are people who are willing and able to travel to the facility where the trial is conducted. People who join trials are sometimes more health conscious than the average person, or more likely to be from an urban versus a rural area. Participants also tend to be less diverse, or from different socioeconomic backgrounds than the general public. We want to remove that bias from the trial. That allows us to study people who are more likely to be the future users of Lark, so that the results that we’re obtaining are applicable to the general population. We want to make sure that we’re reaching the people who we know will be the users of our program.
Are there other benefits of a decentralized trial?
We are also hoping to connect a lot of fragmented information. We want to link laboratory results with clinical findings, and with the user’s every day well-being measures. That is why we really have our eyes on this decentralized clinical trial.
Home is where the trial is
February 7, 2022

When Curavit Clinical Research launched in December 2019, the startup was looking to blaze a new trail in the clinical trial space. Quite simply, they added a “V” before the traditional “CRO,” and positioned themselves as the “first virtual contract research organization (VCRO).”
The timing could not have been more apt — or more of a challenge. The pandemic had supercharged the move toward decentralized clinical trials (DCTs), including virtual trials, and furthered already-strong regulatory tailwinds, Dave Hanaman, Curavit’s president and chief commercial officer, says. But it also created logistical challenges and upended the company’s planned roll-out strategy.
“We fully expected that the decentralized market, while small, was going to grow at a steady pace and a lot of that would come from Big Pharma,” Hanaman says.
But trials at large companies had suddenly come to a screeching halt.
“Big Pharma was suddenly working from home and if you weren’t doing COVID trials, but you were in clinical research, then you were sitting at home, and you were planning things for post-COVID,” Hanaman says.
Curavit pivoted quickly, focusing even more of its attention on small and midsize companies.
“Big Pharma has the luxury to be patient and that’s appropriate. Small, midsized biotech start-ups don’t,” he says. “They’ve got venture capital, they’ve got a binary equation on success. They’re either going to be successful or they’re not.”
Many early adopters of DCTs have historically been bigger companies, in large part because they have the resources to make the transition. But it’s actually smaller and midsize biotechs that stand to benefit disproportionately from decentralization, Hanaman says.
For these companies, DCTs have provided a lifeline to keep research moving.
An outsized benefit
For smaller pharma companies, DCTs can mitigate a number of challenges — from recruitment struggles to global deployment challenges. Decentralization can also help expedite trials, allowing them to adapt quickly in response to data.
Drugs and diagnostics at small to midsize companies typically target a focused, distinct audience, and often focus on rare diseases, Hanaman says.
“Decentralized trials allow them to recruit from all over the country or potentially all over the world,” Hanaman says.
Decentralized technology can also help facilitate global, multi-site trials, says Alison Holland, executive general manager, Digital and Decentralized Solutions for Medable, a software provider for decentralized trials.
“Very few companies, including the small to midsize, are working in just one jurisdiction,” Holland says. “They’re looking for broader exposure, broader registrations.”
According to Holland, decentralized trial providers can help to plan for site-specific needs, accommodating for local data collection, privacy, and regulatory requirements, which can vary by country.
DCT technologies and devices can also speed trials, allowing for more data collection in a shorter period of time, with greater efficiency and reach, Hanaman says. Researchers can then interpret this data more quickly and accurately, which can enhance patient safety, and encourage participation and participant satisfaction. For example, if a red flag is detected on a daily measure of blood pressure, heart rate, temperature or weight, the subject can be brought in for evaluation quickly.
DCTs also make trial participation more appealing because they require less hassle and travel to research sites. Easing the process helps to encourage those who might otherwise be reluctant to participate. This is particularly true for people who are in poor health, such as oncology patients.
“If home is a relaxing, safe environment for them, they might appreciate the option to be there,” Holland says.
Understanding the challenges
There are also some inherent challenges for small to midsize biotechs that chose to go the decentralized route. First, DCTs require an up-front investment, not only in terms of dollars, but of time, focus and energy, Hanaman explains. Making the leap ultimately enables these organizations to run more efficient trials going forward — but they have to get over that initial hurdle first.
Second, deviating from traditional research practices can bring risk and scrutiny.
“If everybody adopted DCT technologies and processes then everybody would start to benefit. But when one company does it, they expose themselves, correctly or incorrectly, to be challenged on their results,” Hanaman says.
For others, the main challenge is overcoming paralysis. Many companies are interested in DCTs, but simply don’t know where to start.
“It’s such an overwhelming thing,” Holland says, explaining that companies often don’t know how to adapt technology to their individual study.
For all of these reasons, many smaller organizations choose to dip a toe into the water rather than jump in all at once.
“A vast growing middle section of trials are hybrid, and that’s really where companies can and should be,” Hanaman says. “You don’t have to be all in on one or another. One can say, ‘What are the technologies that work for us? How do we design our trial from these digital first principles, and then add in traditional components in a way that is better for patients, better for research, better for outcomes?’ And that often is in this hybridized space.”
Strategies for successful implementation
In order for decentralization to work, it has to be implemented correctly. Some companies try to design a trial in a traditional way and then shoehorn in technology, Hanaman says. Instead of being more convenient for participants, the end result is a clunkier trial that increases the burden because participants still need to go to the site, but they also need to learn the technology.
Instead, companies should take a more comprehensive planning approach.
“I would encourage everyone to not to get overwhelmed by the breadth of what a DCT could be and to think about their protocol,” Holland says. “What’s the scientific question that their protocol is trying to answer?”
In particular, she advises that companies ask how they can answer that question in a more digital fashion, that allows for choices for the site and the patient.
Both Hanaman and Holland suggest consulting with DCT support providers as early as possible in the trial design process. This can help determine how technology can best be used to achieve trial aims. Ultimately, successful DCT adoption requires a focus on one core goal, Holland says.
“DCTs aren’t about no bricks and mortar, or no sites — it’s about amplifying the relationship between the site and the patient,” she says. “If we approach it from the perspective of ‘How do we engage patients with their clinicians and caregivers more?’ then it really opens up a huge opportunity for us to transform how we deliver healthcare and how we collect data.”
Oncology: Surprising Therapeutic Area Ripe for Decentralized Research
February 7, 2022

Oncology represents the largest research area globally, with 6.5% annual growth from 2000 to 2020 compared to 3.6% for nononcology drugs in development. At the same time, oncology trials face unique challenges including patient enrollment and retention problems, complex trial designs across more sites, larger data sets, longer durations, and more protocol deviations (to name only a few). In fact, the three phases of oncology trials last almost 12 years, on average, compared to 8 years for nononcology trials. And oncology trials generate a much higher volume of data: 3.1 million data points per protocol in phase 2 oncology compared with 1.9 million in nononcology.
It’s no surprise that, as of June 2021, only 5% of the 4,576 trials utilizing DCT strategies are oncology studies. Various explanations for this lag may include the type of investigational product, the need for invasive tests and scans, and the uncertainty surrounding the effect of remote assessments on data quality. However, a well-designed DCT that considers regulatory and operational concerns can not only overcome these issues but also improve research performance, data quality, and speed.
Wrong Assumption: Cancer Trial Patients Prefer In-Person Visits
Many cancer patients would prefer to stay home. For instance, patients diagnosed with acute myeloid leukemia—a cancer of the blood and bone marrow that progresses rapidly—juggle many physical and psychological side effects from the time they receive initial treatment through their post-hospitalization course. Prolonged symptom management, often involving nausea and fatigue, makes outpatient visits particularly challenging. Follow-up oncologist appointments are already time-consuming and may include blood transfusions, intravenous medication delivery, and comorbidity management. Tacking on additional research assessments before patients can go home may be more than they can bear.
DCT technologies enable remote monitoring so ailing cancer patients can remain in the comfort of their homes and reduce the burden of in-person visits, in turn, attracting more trial participants. Continuous remote monitoring provides the added benefit of better real-world data.
Pete, a middle-aged survivor of acute lymphoblastic leukemia, endured an arduous, three-year chemotherapy course. Three months into his treatment, he entered a clinical trial using blinatumomab, which was taken in parallel with his chemotherapy. Within just one month, his leukemia disappeared completely, but due to risk of recurrence, Pete underwent three more cycles of trial drug. Today, he sees considerable value in a DCT approach during the maintenance and monitoring phases, which will last for the next three years.
“I do televisits with my oncologist now, which is much easier,” said Pete in an interview for this article. “You can’t replace in-person visits in the early stages of a trial, but virtual technologies can ease the burden long-term.”
Digital Therapeutics Sector Projected to Grow Exponentially
January 24, 2022

As the digital therapeutics/software as a medical device sector continues its significant growth, clinical trials for the products are projected to expand logarithmically.
The space is seeing a big transformation from merely following patient symptoms to serving as interventions in a growing number of areas, according to Mark Opler, chief resource officer for directing research and development at WCG MedAvante-Prophase.
“This used to be, I would say, almost a fringe category of potential treatments. It’s moved considerably from symptom tracking to intervention,” Opler told CenterWatch Weekly. “There is an ever-widening array of conditions and symptoms that digital therapeutics are intended to treat. Mood disorders, particularly depression, anxiety, those have been traditionally thought of as the core target categories for digital therapeutics, but as time goes by, we’re seeing applications to psychosis, to trauma and to other diseases, including attention deficit and related conditions.”
The FDA has already approved a number of digital therapeutics products. These include Akili Interactive’s EndeavorRx, an ADHD videogame treatment for children, NightWare’s self-titled product that uses an AppleWatch and iPhone to disrupt nightmares without disturbing sleep and a trio of Pear Therapeutics apps for chronic insomnia, opioid use disorder and substance use disorder.
Digital therapeutics can also be developed to serve as coaching tools to help improve certain behaviors. While some are intended to serve as standalone products, others are being developed for use in combination with drugs or other medical devices. The sector’s growth is predicted to grow to $12.1 billion by 2026.
Because patients are using a piece of software, not simply taking a drug, determining what will be used as the placebo can be a taller order. Some companies come up with “inactive,” nontherapeutic software to serve as the placebo, while others develop games or use treatment as usual for patients in the placebo control group.
But according to Opler, it may be more fruitful to concede that this method of blinding “may be on some level challenging, if not impossible” and go another route: using an evaluator that has as few ties as possible to the trial beyond assessing patient symptoms, an avenue for blinding that’s gained greater traction in digital therapeutics trials.
“What’s transpired instead when you want to evaluate efficacy in an objective way in a digital therapeutics study is to have a fully independent and blinded evaluator, someone who is blinded as much as possible to the treatment and the study design, and whose only contact with the patient is evaluating their symptoms,” Opler said. “It’s tough to find the sugar pill equivalent in a digital therapeutics trial. Blinding the evaluator, keeping them independent from other aspects of conduct of the study, is another route to ensuring that the evidence we gather is rigorous and will be acceptable to the larger community.”
Endpoints are another big issue for digital therapeutics trials, according to Dave Hanaman, president and chief commercial officer of Curavit, a virtual CRO…
Curavit Earns HIPAA Seal of Compliance
January 10, 2022

BOSTON – January 5, 2022— Curavit Clinical Research announced today that it has taken all necessary steps to prove its good faith effort to achieve compliance with the Health Insurance Portability and Accountability Act (HIPAA). Through the use of Compliancy Group’s proprietary HIPAA solution, The Guard™, Curavit can track its compliance program and has earned its Seal of Compliance™.
The Seal of Compliance is issued to organizations that have implemented an effective HIPAA compliance program using The Guard. HIPAA is made up of a set of regulatory standards governing the security, privacy, and integrity of sensitive healthcare data called protected health information (PHI). PHI is any individually identifiable healthcare-related information. If vendors who service healthcare clients come into contact with PHI in any way, those vendors must be HIPAA compliant.
Curavit has completed Compliancy Group’s Implementation Program, adhering to the necessary regulatory standards outlined in the HIPAA Privacy Rule, Security Rule, Breach Notification Rule, Omnibus Rule, and HITECH. Compliancy Group has verified Curavit’s good faith effort to achieve HIPAA compliance through The Guard.
“HIPAA compliance is imperative for clinical research, increasingly so as the clinical trial model becomes more decentralized,” said Joel Morse, co-founder and CEO of Curavit. “As a virtual contract research organization that designs clinical trials from digital first principles, we take patient privacy very seriously, and have built our always–audit-ready platform on validated technologies that support our HIPPA compliant processes.”
According to a statement by Compliancy Group, “Clients and patients are becoming more aware of HIPAA compliance requirements and how the regulation protects their personal information. Forward-thinking providers like Curavit choose the Seal of Compliance to differentiate their services.”
About Curavit
Curavit Clinical Research is a virtual contract research organization (VCRO) that designs and executes Decentralized Clinical Trials (DCTs) from digital first principles. Founded by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, minimizing the need for physical infrastructure and travel while increasing data quality and reducing patient burden. Curavit brings together the world’s leading researchers, enrolls previously underrepresented and underserved patient populations, and applies machine learning to health and social engagement information to recruit participants. For more information, visit www.curavitclinicalresearch.com.
Media Contact: Lisa Barbadora (610) 420-3413 lbarbadora@barbadoraink.com
PM360 Presents the 2021 Innovators
December 13, 2021

Innovation. Transformation. Change. Adapt. These words and all their synonyms were repeated ad nauseum during these past two years as people, companies, organizations, and industries were forced to make drastic changes in the face of a global pandemic. As Rajiv Sodhi, COO, Microsoft India, said, “Innovation is no longer an option, but a necessity.” That was in relation to a Microsoft-IDC study in which 77% of businesses in India said that innovation is now a “must” for them to respond quickly to market challenges and opportunities.
Of course, this isn’t an issue isolated to just one country or one industry. According to BCG’s April 2021 report, “Overcoming the Innovation Readiness Gap,” 75% of the 1,500 global executives surveyed across all industries said that innovation is top-three priority at their company—a 10 percentage point increase from 2020, which is the largest year-over-year increase in the 15 years of BCG’s Most Innovative Companies survey. Furthermore, more than 60% of companies plan to boost investment in innovation, with one-third of them planning to do so significantly.
If these companies stick to their word, we may be entering a new age of innovation. That may be a sight to behold because in our industry alone, the innovations over the past two years have been significant. Yes, that includes COVID-19 vaccines developed in record time, but it’s more than that. Healthcare delivery, clinical trials, commercialization efforts, organization management, and much more were all reimagined to work better during a pandemic and even well into the future as we embrace our next normal.
For the past decade, our annual Innovations Issue has served as your guide to all things new and next in the industry to better prepare you for the future. As innovation only grows more crucial, so does this guide. From hundreds of submissions, we picked the most gamechanging innovations you need to know about in the following categories:
- Companies (any organization developing new ways to push the industry forward)
- Divisions (new sectors formed to address a particular problem facing the industry)
- Startups (companies less than five years old pioneering new avenues in healthcare)
- Products (software, apps, programs, and anything else designed to improve how those working in the industry do their jobs)
- Services (compelling offerings that help the industry tackle new challenges)
- Strategies (never-before-tried approaches that are changing how the industry operates)
These selections are meant to aide in your own innovation journey with potential partners, worthwhile offerings, and inspiring ideas that can help you stay ahead of the game in a world that has now made innovation one of its top priorities.
Advantages of Digital Decentralized Trials with Curavit’s Dave Hanaman | Interview
20 Years in the Making: Reflections and Predictions
November 15, 2021

NEXT FRONTIER: The next frontier for clinical trials is in-silica research, also – confusingly – called virtual trials. In this future of research, “subjects” are computer models, data is real world data (RWD), and the experiments are conducted through computation – not human observation and measurement. There are already some good examples of this. The Economist recently reported on the one from the UK, but it will be a very long time before this is a significant disrupted to clinical research.
Curavit Clinical Research announced the appointments
As seen in – Applied Clinical Trials
October 20, 2021
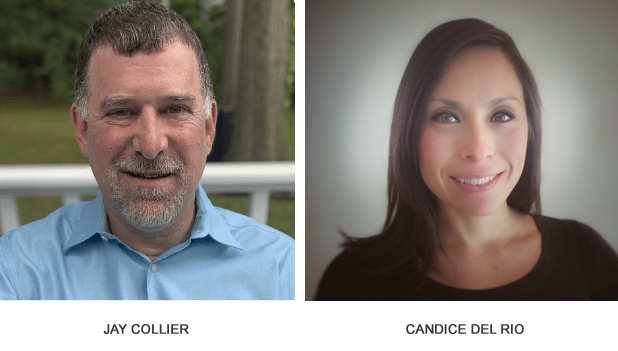
Curavit Clinical Research announced the appointments of Jay Collier, as Chief Operating Officer, and Candice Del Rio, as Director of Clinical Operations.
Decentralized Clinical Trials: What Therapeutic Areas are Ripe for All-Virtual?
As seen in – Applied Clinical Trials
October 20, 2021

Before the pandemic, a December 2019 Industry Standard Research survey found that 38% of pharmaceutical sponsors and contract research organizations (CROs) expected virtual trials to be a major component of their portfolios, and 48% expected to run a trial with most activities conducted in participants’ homes. One year later when attendees at McKinsey’s Clinical Operations Roundtable were asked the same questions, the responses were 100% and 89%, respectively.
Today, most are asking what trials and what aspects of trials can be effectively decentralized and to what degree. Fully virtual or decentralized clinical trials (DCTs) typically handle all enrollment processes and assessments in a patient’s home, enabled by end-to-end digital tools and involve the self-administration of medicines. This model is gradually migrating from smaller, early-phase and post-approval studies toward larger pivotal trials, such as Otsuka and Click Therapeutics’ landmark fully remote clinical trial to investigate the effectiveness of digital therapeutics in reducing symptoms in adults diagnosed with major depressive disorder (announced in Feb 2021).
In the near term, sponsors, investigators, and CROs expect fully virtual trials to remain limited to a narrow set of use cases, such as a well-characterized drug with few adverse events in a mild indication, with end points suited to remote measurement. Long-term, however, fully virtual trials will be more widespread—especially in certain therapeutic areas such as rare disease, mental health, central nervous system, neurodegenerative and others that require patient populations that can’t physically travel or don’t live near a site.
Ultimately, the therapeutic area alone shouldn’t determine a trial design. Rather, each trial should be designed for-purpose and centered on patients. The target patient population, treatment, and indication will primarily determine whether a trial is fully virtual, hybrid or a traditional site-based trial. Even so, there are defining patient population characteristics in many therapeutic areas that can make some studies more likely candidates for all-virtual research.
Here are five therapeutic areas that are particularly apt for an all-virtual research approach, and that can serve as an entry point for hesitant sponsors interested in exploring this growing DCT model.
Diabetes—More than one in 10 Americans have diabetes and one in three or 88 million adults are prediabetic. Given the disease’s prevalence and its widespread geographic reach including many rural areas, diabetes is ripe for fully virtual research. Blood glucose values can be monitored continuously with wearable devices attached to the patient’s skin and automatically uploaded to a central platform in the cloud for easy access by trial investigators, sponsors, and the patients themselves.
In addition, the propensity of patients with Type two diabetes to be elderly or struggle with obesity can make it difficult for patients to travel to trial sites. These patients often have vascular problems which also can also hinder mobility. Further, diabetes is rampant in certain demographics such as Native Americans who are twice as likely to have diabetes as whites and often live in remote rural areas far away from the nearest clinician. Virtual trials bring lifesaving treatment to these patients and further the development of treatments that reflect the unique needs of a more representative population.
Cardiovascular—With wearable devices, including Apple watches, that monitor increasingly more sophisticated and wider range of cardiovascular endpoints remotely, research focused on cardiovascular diseases are apt for a fully virtual trial design. These devices accurately monitor and measure cardiac events and catch issues, such as atrial fibrillation (a common type of sustained cardiac arrhythmia) and ventricular tachycardia (abnormally fast heart rate) to alert the patient and remote physician in real time. Even some clothing items, such as bras, have sewn-in heart monitors! There are other devices that can be worn continuously for months at a time to capture more sophisticated measurements and automatically send data into the cloud. The same is true when it comes to managing blood pressure.
Like diabetes, cardiac patients are in all corners of the world and often many hours from central research sites and—due to their condition—may have mobility challenges and concerns. Virtual trials extend access to the millions living with heart disease and high blood pressure. Further, the data gained from continuous and multiple-symptom monitoring of cardiac patients is dramatically more useful in comparison to the less-reliable, one-hour, single-symptom testing completed at a site once a month or every few months. Heart arrhythmia often occurs only intermittently so it may not be picked up at the occasional site visit. Today’s wearable devices monitor blood pressure, heart rate and rhythm, and oxygen saturation levels as well as activity level (steps taken) so researchers can superimpose different measurements depending on what endpoint is being studied or combine multiple measurements for more meaningful information.
Central nervous system (CNS) diseases—Parkinson’s Disease, Multiple Sclerosis, Alzheimer’s disease, and other CNS diseases may dramatically impact patients’ mobility as well as hamper caregivers’ ability to bring affected loved ones to frequent clinician visits. All-virtual trials open these patients up to potential opportunities they might not otherwise ever have for a treatment.
Like cardiac wearable devices, there are an increasing number of new technologies that allow researchers to measure novel endpoints of patients in the comfort of their own homes and in more realistic life settings outside of a doctor’s office. Devices can continuously measure number of hand tremors per minute, for example, so a novel endpoint could be the reduction of hand tremors which was not as easily studied in traditional trials.
An electroencephalogram (EEG) is a widely used non-invasive method for monitoring the brain but has historically been a large and bulky technology, restricted to the monitoring of subjects in a lab or clinic while they are stationary. Today, we can use a wearable EEG, which overcomes these limitations and allows the long-term, non-invasive recording of brain signals at home.
Neuromuscular trials—Like patients with CNS disorders, patients struggling with neuromuscular diseases, including Duchene Muscular Dystrophy may have severe mobility challenges that make it difficult to make regular clinician visits. Fortunately, there are advanced activity monitors that do not interfere with movement on these patients such as ankle bracelets that can record various measurements continuously to, say, show how much activity a person takes part in over a period. Red Nucleus Clinical’s iTakeControl platform is a clinically approved solution that enables HIPAA-compliant video assessments of patients, live video research visits and audio recording to provide richer audio/visual data that is also auditable for compliance purposes.
Insights into Defining Decentralized Clinical Trials
As seen in – Applied Clinical Trials
October 20, 2021

Decentralized Clinical Trials (DCTs) have taken the main stage in the clinical trials industry, which was significantly facilitated during the pandemic. However, similar to the initiation of risk-based monitoring (RBM), the concept of DCTs is at an infancy stage, and many enterprises are competing to make their mark in the field. This prompted the formation of the Decentralized Trials & Research Alliance (DTRA) to help better define and advance DCTs. In this article, Dave Hanaman, Co-founder of Curavit, will discuss his perspectives on DCTs.
Moe Alsumidaie: What is a Virtual CRO (VCRO)?
Dave Hanaman: Co-founder Joel Morse and I conceived the company from our experience at C3i, where we spent 20 years at the intersection of digital technologies and clinical research. We saw this space evolving for years and wanted to disrupt research by positively applying technology in new ways. So we launched Curavit officially in November 2019 and became the first virtual CRO—a contract research organization dedicated exclusively to designing and executing decentralized clinical trials.
As a VCRO, Curavit runs fully decentralized trials from start to finish and acts as a virtual site, managing the decentralized components of a hybrid clinical trial. We leverage industry-leading digital technologies, devices, and our cloud-based DCT platform to centrally capture, aggregate, manage, and analyze trial data for sponsors. Curavit also brings specialized therapeutic expertise for decentralized trials to ensure the most proficient minds and the best technologies are applied to every research study.
As a VCRO, Curavit runs fully decentralized trials from start to finish and acts as a virtual site, managing the decentralized components of a hybrid clinical trial. We leverage industry-leading digital technologies, devices, and our cloud-based DCT platform to centrally capture, aggregate, manage, and analyze trial data for sponsors. Curavit also brings specialized therapeutic expertise for decentralized trials to ensure the most proficient minds and the best technologies are applied to every research study.
DH: Yes, and the technology is catching up to the vision. In 2007, Veeva introduced cloud-based CRM to an industry desperate for lower-cost technology models because so many major brand-name blockbuster drugs were coming off patent. Veeva’s well-touted success is an example of the right solution at the right time. Decentralized trials are similarly destined, supported by developments in IoT, wearables, and big data. People have been working to make DCT a reality for years, but the technology is finally maturing and readily available while the industry is calling for a greater focus on patients and access to trials for all. So once again, we have a case of the right solution at the right time.
MA: Are there concerns around data privacy and what precautions is Curavit taking to protect it, especially now where the U.S. and many Western nations are under attack by foreign hackers. What can be done to address those concerns using a DCT model for research?
DH: From banking to life sciences, every industry is extremely concerned about protecting data. As in most things, there are tradeoffs. Decentralized trials that do not involve sites can be an advantage in limiting data risk. DCTs can be much more secure in many ways because you can centralize data in very safe, modern cloud systems. That is what Curavit is doing.
Curavit’s platform has been purpose-built for decentralized trials with proven, industry-leading software. HIPAA compliance and validation are built into the individual tools as well as the overall platform. No corners were cut in terms of applying modern cyber defenses.
MA: Part of Curavit’s vision is to make research more accessible across all the demographics. How are you expanding clinical trials to those demographics through DCTs?
DH: First, DCT technologies and processes are fundamentally more suited to reaching previously underserved or underrepresented patient populations. It’s easier to expose more people to the opportunity to participate in research across social media, digital communities, and websites supporting specific diseases or conditions.
Second, and more specifically, DCTs leverage community-based outreach. For example, we partner with Clinispan out of North Carolina whose purpose is to recruit underserved populations. Par 80 in Boston partners with community health centers serving minority populations. These efforts reach out to minority populations to include those who distrust or have not been previously exposed to research.
Third, we have had ongoing discussions with a global pharmaceutical company interested in Native American populations that embody two distinct underserved groups: indigenous and rural populations.
MA: Where do you see DCTs going in the next ten years?
DH: Optimistically, in 10 years, we won’t think of DCTs as unusual because the technologies and processes will be commonplace. DCTs won’t be any more novel than computerized businesses are today.
Most data capture will be in the cloud a decade from now, and DCTs will enable a more burdenless patient research experience. To clarify, that doesn’t mean face-to-face interactions with physicians will go away. Even in complex therapeutic areas like oncology, there’s plenty of opportunities to use digital technologies to gather new data and reduce patient burden. We won’t think of DCTs as a distinct subset. In 2031, DCTs will have disrupted clinical research in profound ways that are better for all patients, better for all sponsors, and ultimately better for public health.
Decentralized Clinical Trials Poised to Expand Their Reach
October 19, 2021

An understanding of human nature suggests that in a post-COVID-19 era for clinical trials, the pendulum may temporarily swing away from the increased adoption of decentralized clinical trials (DCTs) and hybrid approaches that we’ve been witnessing and revert to something more closely resembling the traditional, in-person trial conduct practitioners and patients had been used to before 2020. However, Dave Hanaman, chief commercial officer for Curavait Clinical Research, sees “steep continued growth” in the years to come for new technologies and approaches that he believes can significantly advance the quality and reach of clinical trials.
“DCTs present a new opportunity to meet patients wherever they are,” says Hanaman. The approach they offer represents “an effective way to bring the trial to the patients,” he adds.
Acknowledging some industry “growing pains” as hybrid trials and DCTs have begun to take hold, Hanaman warns that some hybrid approaches are “the worst of both worlds,” with too heavy a physical footprint and overuse of technology.
However, Hanaman sees “strong levels of adoption” for hybrid trials in the next five to 10 years. “Much of the resistance has dropped,” he explains. “I think their use will be taken for granted” in the years to come, he says.
Hanaman is excited, too, about how hybrid trials and DCTs can expand the reach of clinical trials. In addition to traditionally underserved patient populations like African Americans and Hispanics, Hanaman notes the new technology and approach could improve trial access for native American and rural white populations. “Native American populations are often very far away from physical research sites,” he notes.
Further, internet coverage, long an obstacle to increased use of telehealth and DCTs, has improved in many of even the most geographically remote parts of the United States, Hanaman says.
DCTs and hybrid trials represent “a tremendous opportunity for patients and science,” he says. “I see so much more enthusiasm for [such approaches] to be included in trial design, and [they] will help us better reach the patients we’ve been missing.”
Meet The Disruptors: Dave Hanaman Of Curavit Clinical Research On The Three Things You Need To Shake Up Your Industry
October 11, 2021

As a part of our series about business leaders who are shaking things up in their industry, I had the pleasure of interviewing Dave Hanaman.
Dave Hanaman is co-founder, president and chief commercial officer of Curavit Clinical Research, a virtual contract research organization (VCRO), that designs and executes decentralized clinical trials (DCT). He is a proven entrepreneur, operator, and board director with successful, strategic exits to public companies. Founder of C3i, a Business Process Outsourcing (BPO) healthcare provider that was sold to a Fortune Global 500 company in 2018, Dave developed and led its sales, marketing, product development, and alliance strategies. Dave serves as a board member and advisor to several start-up and growth-stage companies in healthcare and technology. When not working, he enjoys spending time in the world’s mountains and oceans. He passes on his passion for the wilderness as an instructor for the National Outdoor Leadership School, where he teaches leadership to groups as diverse as the US Army, the US Forest Service, and Google. He graduated from the University of California at Berkeley and served as a deployed U.S. Navy intelligence officer.
Thank you so much for doing this with us! Before we dig in, our readers would like to get to know you a bit more. Can you tell us a bit about your “backstory”? What led you to this particular career path?
At my previous company, my co-founder, Joel Morse, and I spent 20 years at the intersection of clinical research and digital health technology, working with the world’s leading pharmaceutical companies. We became very interested in the ways that these technologies and processes could benefit patients, researchers, and healthcare organizations. I am very happy to be working with him and several other former colleagues now at Curavit, which launched in 2019.
Can you tell our readers what it is about the work you’re doing that’s disruptive?
At Curavit, we are designing and executing decentralized, or “virtual,” clinical trials, which are the application of digital technologies, wearable devices, internet-of-things, innovative trial design, and supportive regulation to increase the speed and fidelity of clinical research, while simultaneously attracting previously undeserved patient populations.
Can you share a story about the funniest mistake you made when you were first starting? Can you tell us what lesson you learned from that?
While not exactly a “funny” story, I have one that was completely unexpected. We announced Curavit at a major clinical research conference in January of 2020, when the industry was breathlessly predicting that 10% of all trials would be “virtual” in ten years. No one foresaw the impact of the pandemic and the unprecedented forced adoption of decentralized trials within months. We found ourselves suddenly accelerating toward our goals with massive tailwinds, but also buffeted by lots of noise and turbulence from the hype. We again learned the lesson that “the first casualty of battle is the plan,” and that you have to stay committed to the outcome while adapting to the things you can’t control.
We all need a little help along the journey. Who have been some of your mentors? Can you share a story about how they made an impact?
I learned so much from the men and women I served with in the Navy. From my Marine drill instructor, to the commanding officers I worked for, to my squadron mates and colleagues, they continue to inspire and motivate me every day. And of course my family; I have always enjoyed the full support of my wife and sons through the good, bad, and most of all uncertain times associated with being an entrepreneur.
In today’s parlance, being disruptive is usually a positive adjective. But is disrupting always good? When do we say the converse, that a system or structure has ‘withstood the test of time’? Can you articulate to our readers when disrupting an industry is positive, and when disrupting an industry is ‘not so positive’? Can you share some examples of what you mean?
I believe that “disruption” is a neutral word and that in practice it usually results in both positive and negative outcomes, depending on one’s perspective. For decentralized clinical trials (DCT), a good example might be the impact on sites. Are DCT’s “site-less” trials? Sometimes. Does that mean that some sites are negatively impacted by DCTs? Yes. But the flip-side of that may be reducing patient burden and increasing diverse enrollment, and those are positives. Furthermore, as with most disruption, it won’t be that simple. In this example, I believe some sites will prosper by embracing DCT technologies and processes, benefiting themselves as well as patients.
Can you share 3 of the best words of advice you’ve gotten along your journey? Please give a story or example for each.
One of our sales people once said, “If you’re explaining, you’re losing!” This means your value to your customers has to be clear and compelling.
An early advisor to my first company said, “Sometimes, you gotta tell ’em the baby is ugly.” In other words, don’t be afraid to see and speak the truth.
And recently, one of our current investors (and an advisor to our company) reminded me that my ultimate job is to detach and put myself in our customers’ shoes. Our success depends on our ability to meet and exceed customer needs and expectations over the long term.
We are sure you aren’t done. How are you going to shake things up next?
Curavit is my “next” right now. We are in our formative stage and are building out our team. We have an opportunity to do a lot of great work for the next few years and help shape the future of clinical research. That’s plenty for now, so no clear plans for a “next thing” just yet!
Do you have a book, podcast, or talk that’s had a deep impact on your thinking? Can you share a story with us? Can you explain why it was so resonant with you?
I usually read fiction or philosophy every night, even if only for a few minutes. In the gym or the car, I’ll listen to podcasts and audiobooks on a broad (and non-business-specific) array of topics often touching on history, exploration, geopolitics, and leadership. Right now I’m listening to the audio book “A Hunter Gatherer’s Guide to the 21st Century,” and just finished a 9/11 retrospective podcast series on Michael Morell’s Intelligence Matters podcast. Apropos of this interview, a keynote presentation that still resonates with me was one I heard years ago by Dr. Clayton Christensen on his seminal book, “The Innovator’s Dilemma.” That talk still informs my thinking around our strategy at Curavit today.
Can you please give us your favorite “Life Lesson Quote”? Can you share how that was relevant to you in your life?
I love quotes, and keep a list of my favorites. In this context, I’ll pick Theodore Roosevelt’s famous words found in “Man in the Arena.”
“It is not the critic who counts, not the man who points out how the strong man stumbles, or where the doer of deeds could have done them better. The credit belongs to the man in the arena, whose face is marred by dust and sweat and blood, who strives valiantly…who knows the great enthusiasms, the great devotions, who spends himself in a worthy cause, who at the best knows in the end the triumph of high achievement, and who at the worst, if he fails, at least fails while daring greatly, so that his place shall never be with those cold and timid souls who have never known neither victory nor defeat.” — Teddy Roosevelt
The most rewarding aspect of being an entrepreneur for me is commitment in the face of adversity and uncertainty which TR captures so well in that speech.
You are a person of great influence. If you could inspire a movement that would bring the most amount of good to the most amount of people, what would that be? You never know what your idea can trigger.
It would simply be to encourage people who are considering a different path to take the risk of engaging in a new venture. Of course we should plan and prepare, but eventually one simply has to make a leap of faith.
How can our readers follow you online?
You can find me and the rest of the Curavit team and follow our progress at https://www.linkedin.com/company/curavit/ and https://www.linkedin.com/in/davehanaman/.
This was very inspiring. Thank you so much for joining us!
Curavit Clinical Research announced the appointments
As seen in – outsourcing-pharma.com
October 7, 2021

Decentralized Trials & Research Alliance Grows, Partnerships in Site Conduct, Trial Diversity, More
As seen in – clinicalresearchnewsonline.com
October 7, 2021

Curavit Clinical Research, a virtual contract research organization (VCRO) that designs and executes decentralized clinical trials (DCTs), announced today that it has joined the Decentralized Trials & Research Alliance (DTRA) to further the advancement and adoption of decentralized clinicals. Curavit Clinical Research has also announced the appointments of Jay Collier, as chief operating officer (COO), and Candice Del Rio, as director of clinical operations. The company also expanded its sales team with the hiring of Chris O’Shaughnessy, as vice president of business development, as well as Troy Hall and Bill Dreyer, as directors of business development. The expansion comes as DCTs continue their steady growth, punctuated by Curavit’s doubling its revenue since 2020.
Curavit joins decentralized trials group, predicts demand will keep growing
October 5, 2021

Curavit has joined the Decentralized Trials & Research Alliance, an industry-backed non-profit organization focused on the promotion of remote studies.
Membership of the group will see Curavit take part in the development of the fast growing the decentralized clinical trials market according to co-founder, president and chief commercial officer, Dave Hanaman.
“DTRA provides a broader platform for Curavit to discuss the innovations and research improvements that we are driving for our clients. Curavit will also have the benefit of collaborating with other innovators to solve new or emerging challenges in a way that is meaningful for the entire industry.”
Demand for decentralized trials has increased significantly in recent years – particularly since the pandemic – Hanaman told Clinical insider and predicted demand would continue.
“Curavit sees demand for DCTs daily in the form of customer feedback. Clients are developing long-term plans to leverage decentralized components in most of their trials. COVID-19 changed the industry’s approach, impacting everything from long-range planning to execution and it doesn’t seem like we are going back to traditional methods.”
He added, “Today, most trial designs have at least on decentralized component included and every large pharmaceutical company Curavit has spoken to over the last year has established a DCT group or team – often referenced as innovation team, trial optimization group, digital team or other similar nomenclature denoting DCTs.”
Curavit was established in 2020 in a bid to tap this growing section of the market. Last month the CRO expanded its sales team in a bid to broaden its service.
Hanaman said, “Curavit is a new company and establishing its sales force from scratch, so we need team members to support the demand. Prior, just Curavit founders have been managing client inquiries and working with clients to ensure long-term satisfaction and responsiveness.
“With our growth, that is not sustainable, as the Curavit leadership also need to devote time to helping to develop unique therapeutic-area-specific solutions for our clients.”
Image: Stock Photo Secrets
Beech Tree Labs Selects Curavit Clinical Research to Push Toward 100% Virtual Clinical Trials
As seen in – trialsitenews.com
September 20, 2021

Beech Tree Labs has developed a novel drug development platform known as resonant molecular signaling (RMS), that aims to address a wide range of illnesses by restoring normal cellular communications and correcting various imbalances triggering problems. The company opted to go virtual for their next Phase 2, FDA-authorized clinical trial to evaluate the effect of Beech Tree’s BT-TML therapy targeting COVID-19 patients. Although many companies have moved to at least some provisional virtual or hybrid approach during the pandemic, Beech Tree Labs took another step toward a permanent move to virtual trials by partnering with Curavit Clinical Research for a fully decentralized trial. The Park City, Utah-based venture has an ambitious plan to disrupt the operation of clinical trials, accelerating timelines and reducing cost while maintaining if not improving quality with improved, patient-centric care.
Move to Decentralized or Virtual Trials more than ‘Flipping a Switch’
Recently, TrialSite writer Joseph Constance assessed the emerging virtual clinical trials landscape particularly in the midst of the COVID-19 pandemic. In an earlier piece, Constance suggested the move to decent…
Chapel Hill startup targets seed funding after working to diversify Novavax Covid-19 vaccine trial
May 16, 2021

A Chapel Hill startup that helped bring diversity to Novavax’s (Nasdaq: NVAX) clinical trials for its Covid-19 vaccine is in the process of raising $250,000 in funding to help it continue to grow.
CliniSpan Health is actively raising seed funding to grow its team of eight to 20 by 2022, said Dezbee McDaniel, the company’s co-founder and head of business development who earned his undergraduate degree from UNC-Chapel Hill.
“We are looking to grow rapidly,” McDaniel said.
The company was started with the goal to bring more diversity to clinical trials, and in January the Novavax trial was the first CliniSpan began recruiting for, McDaniel said. About 17 percent of the Black participants at the Durham clinical trial site and 20 percent at the Chapel Hill site were referred to Novavax by CliniSpan, McDaniel said.
The lack of diversity in clinical trials has been an ongoing problem for years.
In 2020, the U.S. Food and Drug Administration approved 53 novel drugs that had clinical trials with a total of 32,000 patients. Of those patients, 75 percent were white, 8 percent were Black, 6 percent were Asian and 11 percent were Hispanic.
“We are heavily focused on African Americans right now,” McDaniel said. “We want to expand to groups who are Latinx, Native American, rural, women – a lot of other diverse groups who also need access to clinical trials.”
For now, the company is focusing on one population at a time, McDaniel said, because each group has a different history with the medical system and different preferences for how they want to be communicated with.
“With African Americans, the past mistreatment by the health care system is what we have to overcome and that’s something we haven’t directly affected, so it’s difficult to have that conversation sometimes,” McDaniel said.
Having people who reflect those groups do the outreach and recruitment helps make people more comfortable in participating, he said.
The transition to more decentralized trials also helps, McDaniel said.
“If people don’t have to show up physically and they can do it from home, then access for us becomes that much easier of a goal to achieve,” he said.
In addition to the Novavax trial, CliniSpan has partnered with Curavit, a fully virtual clinical trial organization, which perfectly complements CliniSpan’s infrastructure, McDaniel said.
CliniSpan has also signed a licensing agreement for its software with Capstone Health Alliance, a group purchasing organization for hospitals, he said.
“That’s something we’re trying to grow outside of our recruitment services,” McDaniel said. “We’re trying to help other diversity recruitment arms have technological infrastructure to carry out their processes more effectively.”
At the same time, CliniSpan will be helping to recruit for studies that its hospital network participates in, McDaniel said.
CliniSpan, which is led by founder and CEO Dr. David Lipsitz who did his residency at UNC-Chapel Hill, is currently working with five businesses in total and is generating revenue, though McDaniel did not disclose how much.
17 Virtual Clinical Trial Providers to Partner up With
April 7, 2021

Virtual clinical trial providers are your must-partners for any decentralized trial or contingency plan. In March 2020 the FDA encouraged sponsors to assess alternative methods for keeping their trials on track within the existing limitations under Covid-19 quarantine. Remote/virtual trials are no longer just a convenient way to shorten timelines and reduce costs but a rescue solution to ongoing clinical trials. From recruiting participants to designing their virtual experience, remote trial providers and technology can save your data and your budget.
Curavit Clinical Research, has been launched to help realise the potential of decentralised clinical trials
February 20, 2020

A new clinical trials company, Curavit Clinical Research, has been launched to help realise the potential of decentralised clinical trials.
Launched by industry veterans Joel Morse and Dave Hanaman, the new entity will focus on virtual trials.
Curavit Clinical Research co-founder and CEO Joel Morse said: “Curavit is the result of our desire to solve growing challenges to the important work of drug discovery.
“By combining experience, technology, and solid execution, we will bring cutting-edge research to previously untapped and underserved patient populations.”
Curavit Clinical Research is a next-generation clinical trial enterprise that provides decentralised clinical trial execution. It takes a clean-sheet approach to clinical trials, from the design phase to execution.
Optimised on a new virtual model, the company supports patients’ participation from wherever they live.
Curavit Clinical Research chief commercial officer and co-founder Dave Hanaman added: “We are fortunate to have worked with some of the most respected companies and visionary people in the life sciences industry, and are honored by the support we are receiving from them for this effort.”
Global clinical trials market stands at $70bn and continues to grow, while the success rate of trials continues to see a decline. This is often due to lack of enrollment by patients and participation from doctors.
Curavit Raises $5 Million in Series A Funding to Accelerate Growth in Digital Therapeutics Clinical Research
Industry’s first virtual CRO that specializes in decentralized clinical trials achieves key milestones
November 14, 2022
PHILADELPHIA and NEW YORK — Nov. 14, 2022 — Curavit Clinical Research, a virtual contract research organization (VCRO) that specializes in decentralized clinical trials (DCTs), today announced it raised $5 million in Series A funding to accelerate its growing portfolio of research in the global digital therapeutics (DTx) market (projected to grow at a CAGR of 31.4% through 2026). The new funding will be used to expand the company’s DCT capabilities, partnerships, and market adoption of Curavit’s virtual CRO services and platform for prescription and non-prescription digital therapeutics trials.
The funding was led by early-stage technology investor Osage Venture Partners with additional investment from Royal Street Ventures and Narrow Gauge Ventures. It adds to early investments from Curavit founders and individual investors, including industry veterans Clark Golestani, former president of emerging businesses and global CIO of Merck, and former president and co-founder of Veeva Systems, Matt Wallach.
“In order to dramatically lower the cost and increase the speed of clinical trials, the industry must take a new, digital-first approach,” said Wallach who serves on Curavit’s board of advisors. “Curavit was founded by seasoned veterans with deep experience in that sweet spot where technology innovation meets process excellence so I’m proud to play a part in their journey to improve clinical trials.”
“This is an important milestone for Curavit and the industry’s continued momentum in digital therapeutics and decentralized approaches to clinical research,” said Joel Morse, co-founder and CEO of Curavit. “Traditional trial processes and timelines are insufficient – and they limit patient participation. New digital therapeutics are ideally suited for a DCT approach and will help improve access and drive new unique therapies to patients faster.”
The funding brings Curavit’s total capital raised to more than $8 million. Curavit has more than doubled its revenue in 2020 and 2021 and is on the same pace this year. More than half of its customer base are emerging digital therapeutics companies whose clinical research needs align with Curavit’s focus on virtual site services and DCT expertise.
“We are pleased to partner with Curavit on the next phase of their journey,” said Nate Lentz, Managing Partner at Osage Venture Partners. “The COVID-19 pandemic and rapid growth of digital therapeutics has driven a new digital model, where clinical trials are increasingly decentralized and require a new combination of technologies, services, and expertise not available in the marketplace. Curavit’s team and offering are well-positioned to fill this void and become the leading virtual CRO.”
Since its founding in late 2019, Curavit has accomplished key successes on its mission to bring clinical trials of innovative therapies to more patients in the cloud, including:
- Support for important research with digital therapeutics companies, including Swing Therapeutics, Lark Health, Curio, and Sana.
- Strategic partnerships with life sciences digital technology and data providers, including Ripple Science, for its direct-to-patient software platform; ixlayer, to provide easy access to clinical-grade diagnostic lab testing in DCTs; and 1nHealth, for digital patient recruitment and enrollment.
- Hired experienced industry leaders in top positions including Jay Collier as COO, Candice Del Rio as director of clinical operations, and Chris O’Shaughnessy as VP of business development.In other news, Curavit joined the Digital Therapeutics Alliance, whose aim is to broaden the understanding, adoption, and integration of clinically evaluated digital therapeutics with patients, clinicians, payors, policymakers through education, advocacy, and cross-industry collaboration.
About Osage Ventures
Osage Venture Partners (OVP) is a venture capital firm located just outside of Philadelphia, PA. It partners with exceptional entrepreneurs, building the next generation of leading B2B software and tech-enabled services companies. OVP has consistently focused on this strategy since its inception in 2005, making over sixty investments in early-stage B2B companies over that time. For more information, visit OsageVenturePartners.com.
About Curavit
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
Media Contacts:
Lisa Barbadora, +1 (610) 420-3413, lbarbadora@barbadoraink.com
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
BOSTON — Sept. 6, 2022 —Curavit Clinical Research, a virtual contract research organization (VCRO), has entered into a long-term partnership with ixlayer to provide easy access to clinical-grade diagnostic lab testing for decentralized clinical trials (DCTs). ixlayer seamlessly integrates with Curavit’s platform and makes health testing fast and convenient for patients, improving trial enrollment completion rates. Curavit and ixlayer’s first collaboration is for Swing Therapeutics’ trial of an investigational digital therapeutic (DTx) for fibromyalgia.
ixlayer’s patient-centric lab testing program offers multiple testing formats, including flexible digital options, and thousands of testing combinations. The company offers multi-modality sample selection options, such as at-home self-collect, at-home collection assisted (i.e., mobile phlebotomy), and sample collection at a local patient service center. By making health testing easy for patients, Curavit and ixlayer help sponsor organizations improve completion rates and likelihood of patient retention the duration of the trial so organizations get the data they need to facilitate breakthrough discoveries and bring life-changing healthcare innovation to market quickly.
“Curavit is driving innovation in hybrid and decentralized clinical trials, and we are proud to be part of their mission,” said Pouria Sanae, CEO and co-founder of ixlayer. “Lab testing is an integral part of most clinical trials but can burden patients in traditional settings. At ixlayer, we reduce friction for patients and sponsors by digitally simplifying the process and streamlining data collection on the back end.”
Curavit will remotely recruit, screen, consent, and enroll at least 80 participants in Swing’s PROSPER-FM trial and leverage ixlayer’s platform to streamline clinical urine tests to determine participant eligibility. During televisit screening, Curavit’s clinical coordinators seamlessly schedule the patient’s test at one of more than 2,000 conveniently located lab sites in the U.S. through Curavit’s virtual site platform. ixlayer manages all administrative needs, including payment and curating lab results, unburdening patients, resulting in a more positive early-trial experience.
“ixlayer is the leader in flexible lab and home-based testing services,” said Joel Morse, co-founder and CEO of Curavit. “By partnering with ixlayer, we are setting the foundation for a frictionless patient experience in our decentralized clinical trials and greater trial accessibility. As important, together we are improving the efficiency of trials to get important new therapies to more patients faster.”
To learn more about how ixlayer and Curavit are innovating to drive decentralized clinical trials into the mainstream, see us in Boston at DPharm 2022 (Sept. 13-14, 2022) – booth #26.
About Curavit
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
About ixlayer
ixlayer is redefining next-generation consumer experiences for lab testing and better health outcomes.
Retailers, health plans, employers, government entities, and health systems chose ixlayer because our solutions allows them to run health testing programs under their own brand at scale. The ixlayer solution includes an extensive test menu, over 1000 testing options, and omnichannel marketing to end users. ixlayer’s lab independent platform powers health testing programs for partners including the United States Coast Guard, Stanford Health, Salesforce, three of the eight largest national health plans in the US and one of the top retail pharmacy chains. Visit www.ixlayer.com.
Media Contacts:
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
Lisa Barbadora, +1 (610) 420-3413, lbarbadora@barbadoraink.com
Laura Vinci, +1 (212) 529-2236, laura.vinci@finnpartners.com
Digital Patient Recruitment Specialist Partners with Curavit Clinical Research to Speed Patient Enrollment in Decentralized Clinical Trials
1nHealth and Curavit surpass expectations by nearly 3x, enrolling 50 patients in Lark DTx trial in 10 days
October 4, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
BOSTON, Oct. 4, 2022 /PRNewswire/ — Curavit Clinical Research, a virtual contract research organization (VCRO), announced that it is partnering with 1nHealth, a patient recruitment provider, to speed patient recruitment digitally for decentralized clinical trials (DCTs). 1nHealth integrates with Curavit’s DCT platform, speeding trial enrollment and improving retention. Curavit and 1nHealth’s first collaboration is for Lark Health’s trial of an investigational digital therapeutic (DTx) for chronic cardiovascular disease.
Lark’s Heart Health program is designed to help patients manage cardiovascular disease (CVD) risk factors and reduce the rate of future cardiovascular diseases or events. The smartphone-based program uses conversational AI, connected devices, and remote patient monitoring to activate and engage patients by addressing CVD risk factors such as diet, exercise, and tobacco use.
“We are excited to partner with Curavit to improve patient recruitment by simplifying participant identification and enrollment through digital channels,” said Dan Brenner, founder and CEO of 1nHealth. “As a technology-first company, we are closely aligned with Curavit’s mission to bring trials to patients in the cloud. Our partnership will drive faster enrollments and more inclusive trial participation.”
Through targeted ads on key digital media channels (i.e., Google, Reddit, Facebook, Instagram), 1nHealth recruited qualified patients for Lark’s Heart Health trial, surpassing sponsor expectations. In addition, nearly 40% of patients who clicked on an ad went on to complete the pre-screen form. Beyond the early successful 10-day enrollment drive, Curavit and 1nHealth have successfully recruited, consented, and enrolled a total of 150 patients in impressive time.
“During the initial phase of our Heart Health program, we heavily relied on our ability to engage with the right patient, at the right time – not only to track progress but also to ensure the greatest impact on each participant,” said Dr. OraLee Branch, director of clinical studies at Lark Health. “Curavit and 1nHealth’s innovative methods of engaging patients helped us reach our goal. Plus, their fast patient enrollment supports our mission to help patients predisposed to a life-threatening condition or illness.”
Patient recruitment has been a long-time challenge for clinical trials. Globally, 90% clinical trials are delayed due to insufficient patient enrollment. As a result, timelines are typically extended to nearly double their original duration to meet desired enrollment levels. In contrast, 1nHealth enrolls 90% of trials on time using highly targeted, all-digital methods. Together, Curavit and 1nHealth are working to overcome recruitment challenges and help usher in the next generation of decentralized clinical trials.
“COVID-19 initially forced the life sciences industry to try a decentralized approach, and now the indisputable success of DCTs will drive the industry to make it the norm for the foreseeable future,” said Dave Hanaman, co-founder and chief commercial officer at Curavit. “Industry vanguards like 1nHealth bring the kind of innovative tools and thinking that will help speed new therapies to more patients. It’s exciting.”
Lark’s Heart Health program will be commercially available in early Q1 2023. To learn more about Lark and its suite of chronic condition prevention and management programs, please visit them online at www.lark.com.
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
1nHealth fills studies faster by using novel methodologies to deliver high-performing ads across all digital channels. 1nHealth uses AI to help find patients who are simply being missed by other recruitment vendors. 1nHealth works with top CROs, Pharma companies and most of the leading DCT providers, as well as across 40+ TAs, delivering full enrollment for site-based, hybrid, and fully decentralized studies. Visit www.1nhealth.com.
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
ixlayer Partners with Curavit to Enable Convenient Patient Medical Testing Services for Decentralized Clinical Trials
September 6, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
BOSTON — Sept. 6, 2022 —Curavit Clinical Research, a virtual contract research organization (VCRO), has entered into a long-term partnership with ixlayer to provide easy access to clinical-grade diagnostic lab testing for decentralized clinical trials (DCTs). ixlayer seamlessly integrates with Curavit’s platform and makes health testing fast and convenient for patients, improving trial enrollment completion rates. Curavit and ixlayer’s first collaboration is for Swing Therapeutics’ trial of an investigational digital therapeutic (DTx) for fibromyalgia.
ixlayer’s patient-centric lab testing program offers multiple testing formats, including flexible digital options, and thousands of testing combinations. The company offers multi-modality sample selection options, such as at-home self-collect, at-home collection assisted (i.e., mobile phlebotomy), and sample collection at a local patient service center. By making health testing easy for patients, Curavit and ixlayer help sponsor organizations improve completion rates and likelihood of patient retention the duration of the trial so organizations get the data they need to facilitate breakthrough discoveries and bring life-changing healthcare innovation to market quickly.
“Curavit is driving innovation in hybrid and decentralized clinical trials, and we are proud to be part of their mission,” said Pouria Sanae, CEO and co-founder of ixlayer. “Lab testing is an integral part of most clinical trials but can burden patients in traditional settings. At ixlayer, we reduce friction for patients and sponsors by digitally simplifying the process and streamlining data collection on the back end.”
Curavit will remotely recruit, screen, consent, and enroll at least 80 participants in Swing’s PROSPER-FM trial and leverage ixlayer’s platform to streamline clinical urine tests to determine participant eligibility. During televisit screening, Curavit’s clinical coordinators seamlessly schedule the patient’s test at one of more than 2,000 conveniently located lab sites in the U.S. through Curavit’s virtual site platform. ixlayer manages all administrative needs, including payment and curating lab results, unburdening patients, resulting in a more positive early-trial experience.
“ixlayer is the leader in flexible lab and home-based testing services,” said Joel Morse, co-founder and CEO of Curavit. “By partnering with ixlayer, we are setting the foundation for a frictionless patient experience in our decentralized clinical trials and greater trial accessibility. As important, together we are improving the efficiency of trials to get important new therapies to more patients faster.”
To learn more about how ixlayer and Curavit are innovating to drive decentralized clinical trials into the mainstream, see us in Boston at DPharm 2022 (Sept. 13-14, 2022) – booth #26.
About Curavit
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, ultimately bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
About ixlayer
ixlayer is redefining next-generation consumer experiences for lab testing and better health outcomes.
Retailers, health plans, employers, government entities, and health systems chose ixlayer because our solutions allows them to run health testing programs under their own brand at scale. The ixlayer solution includes an extensive test menu, over 1000 testing options, and omnichannel marketing to end users. ixlayer’s lab independent platform powers health testing programs for partners including the United States Coast Guard, Stanford Health, Salesforce, three of the eight largest national health plans in the US and one of the top retail pharmacy chains. Visit www.ixlayer.com.
Media Contacts:
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
Lisa Barbadora, +1 (610) 420-3413, lbarbadora@barbadoraink.com
Laura Vinci, +1 (212) 529-2236, laura.vinci@finnpartners.com
Swing Therapeutics Selects Curavit to Provide Virtual Trial Site Services for Novel Digital Therapeutic Study for Fibromyalgia
June 28, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
BOSTON, June 28, 2022 /PRNewswire/ — Curavit Clinical Research, a virtual contract research organization (VCRO), has been selected by digital therapeutics company, Swing Therapeutics, to be a virtual site for its pivotal trial of an investigational digital therapeutic (DTx) for fibromyalgia. Curavit will remotely recruit, screen, consent, and enroll participants in Swing’s PROSPER-FM randomized clinical trial from across the United States. Curavit will then manage participants throughout the 12-week clinical trial. By eliminating physical and geographic barriers to trial participation and execution, Curavit can scale quickly and improve patient enrollment by at least 10x over a traditional trial, speeding trial execution.
Fibromyalgia is a chronic and debilitating pain condition that affects more than 10 million Americans. It is characterized by widespread musculoskeletal pain often accompanied by fatigue, sleep, memory, and mood disruptions. Swing developed its digital therapeutic with the goal of providing an accessible behavioral therapy option that can be used alongside medication, physical therapy, and other standard-of-care treatments.
“We are focused on getting patient recruitment right,” said Mike Rosenbluth, PhD, Chief Executive Officer at Swing, which recently announced a $10M Series A funding round. “Curavit’s virtual services model enables us to efficiently recruit participants representative of the entire patient population. It solves a huge challenge and will be critical to rapidly develop the evidence needed to bring an effective digital therapy to millions suffering from chronic illness.”
Swing marks Curavit’s 10th DTx client signed in less than six months, a trend in line with a booming global DTx market projected to hit $13.1 billion by 2026, up from $3.4 billion in 2021. Curavit’s decentralized clinical trial (DCT) expertise makes the company well-suited to support prescription and non-prescription DTx studies. Fundamentally, there are no physical logistics with a DTx – no shipping, storing, chain of control, cold storage, or biohazards, plus endpoints can often be captured within the DTx application itself, naturally aligning DCTs with DTx studies.
“Swing is committed to developing scientifically backed digital treatments and evidence to clinically validate their use in the real world, making representative patient participation critical,” said Joel Morse, co-founder and CEO of Curavit. “Our operational model prioritizes patient recruitment and removes geographic boundaries to expand the pool without the expense of physical infrastructure. With zero physical site visits, too, patients are less burdened and more likely to stick with the trial the duration.”
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, and bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across representative populations. Visit www.curavitclinicalresearch.com.
SOURCE Curavit Clinical Research
Ripple Enterprise software to be deployed as part of the digital transformation in clinical trials spearheaded by Curavit
April 12, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
ANN ARBOR, MI- April 12, 2022 – Ripple Science, a digital clinical trial software company, today announced a partnership with Curavit Clinical Research (Curavit) to deploy Ripple Recruit, the company’s newly expanded enterprise software platform, to support several digital therapeutic decentralized clinical trials. Ripple is a natural fit for Curavit’s digital-first disruptive approach to engaging patients, conducting research, and accelerating time to market of new discoveries, especially in the exploding field of digital therapeutics.
“We are hyper-focused on the unique needs of DTx manufacturers, with nearly half of our rapidly growing customer base running studies on novel digital therapeutics,” said Joel Morse, CEO of Curavit, the industry’s first virtual CRO. “Ripple Recruit offers scalable, patient-centric functionality that aligns with our decentralized clinical trial service offering for emerging DTx companies.”
Ripple Enterprise is the world’s only direct-to-patient software platform designed to support decentralized, virtual, and hybrid clinical trials. Designed and audited to 21 CFR Part 11, HIPAA, GDPR and SOC2 standards, Ripple Enterprise enables the entire clinical trial industry to adopt digital clinical trial workflows driving down costs and expanding access to a more diverse pool of patients.
“We’re excited to partner with Curavit which is on the cutting edge of the digital transformation in clinical trials,” said Peter Falzon, CEO of Ripple Science. “This partnership is our largest contract to date and validates our strategic decision to invest in Ripple Enterprise as a response to customer demand for DCT enabling software at enterprise scale.”
About Curavit:
Curavit Clinical Research is a full-service, virtual contract research organization (VCRO), focused on designing and executing digital-first decentralized clinical trials (DCTs). Founded in 2020 by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, bringing trials to patients in the cloud. Curavit’s digital-first DCTs improve timelines, reduce costs, yield real-world data, and increase patient access for therapies more effective across diverse populations. For more information, visit www.curavitclinicalresearch.com.
About Ripple Science:
Ripple Science, a clinical trial technology company, is leading the digital transformation in clinical trials with a direct-to-patient software platform that was built by researchers for researchers. By improving the user experience, increasing regulatory compliance, and further connecting the ecosystem through digital innovation and technology, Ripple delivers real-time transparency, game-changing efficiencies, and more secure workflows & data sharing, concerning all aspects of patient engagement from first contact to last patient visit, whether virtual or in-person.
Ripple Science was named a Top 50 Company to Watch in 2021 by Michigan Celebrates Small Businesses and recognized in 2022 by Purpose Jobs and Cronicle Tech News as one of the fastest growing health tech startup companies in Ann Arbor.
Media Contacts:
Curavit:
Lisa Barbadora
Barbadora INK
lbarbadora@barbadoraink.com / 610-420-3413
Ripple Science:
Anna Falzon
Curavit Named Runner up in BioUtah’s 2022 Entrepreneur & Investor Life Sciences Summit Pitch Competition
April 7, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
SALT LAKE CITY, April 6, 2022 — Curavit Clinical Research, the first virtual contract research organization (VCRO), announced that it was recently named runner up in the 2022 Wilson Sonsini Entrepreneur & Investor Life Sciences Summit (E&I Summit) pitch competition, sponsored by Morgan Stanley. Curavit received the award for its innovative business model and ‘digital first’ approach to democratizing clinical research.
Now in its 7th year, the E&I Summit, presented by BioUtah, BioHive and the PIVOT Center, attracted a record setting 300+ registrants, along with an impressive line-up of distinguished speakers, national and local investors, and numerous Utah life sciences startups.
“We are so happy to be recognized in this capacity by our industry peers and to have had the opportunity to share what we are doing at Curavit,” said Dave Hanaman, Co-founder, President and Chief Commercial Officer of Curavit. “It was an honor to be able to share the stage with so many inspiring companies. Our satisfaction of being recognized by the judges was only overshadowed by the exciting ability to engage with so many innovative entrepreneurs and investors in the dynamic Utah ecosystem.”
The conference featured notable keynote speakers, including Jake Manoukian, Head of Investment Strategy for JP Morgan, who shared insights on market trends and life sciences investment, and Stanford University professor Matt Vassar, who provided a thought-provoking address on “Telling Your Story.”
Out of a total of 21 life sciences companies, Curavit advanced to the popular Pitch Track session through a competitive selection process and went on to win second place after Eliksa Therapeutics.
For being named runner-up in the competition, Curavit was refunded its $1,000 registration fee, which the company donated to BioHive, an organization launched last year to brand, build and bring together the life sciences and healthcare innovation industry in Utah. The funds will be used to support local underrepresented communities, aligned with industry partners to promote K-12 STEM education, workforce development and awareness.
“We are thrilled Curavit sees the value in what we’re doing at BioHive to tell the story of our industry and unite all of the stakeholders for life sciences and healthcare innovation in Utah,” said Katelin Roberts, Executive Director at BioHive. “Their organization works at the nexus of patients, research and industry. Similarly, BioHive seeks to be the hub for our community, and their donation will go toward building our state into a premier life sciences and healthcare innovation ecosystem.”
About Curavit
Curavit Clinical Research is a Virtual Contract Resource Organization (VCRO) that designs and executes Decentralized Clinical Trials (DCT) from digital first principles. Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, eliminating the need for physical infrastructure and travel while increasing data quality. Curavit brings together the world’s leading researchers, enrolls previously underserved patient populations, and applies machine learning to health and social engagement information to recruit participants. The company’s cloud-based, central virtual site is always audit ready. For more, visit www.curavitclinicalresearch.com
About BioUtah
BioUtah is an independent 501(c)(6) trade association serving Utah’s life sciences industry. Its member companies reflect a broad spectrum of the industry with strengths in medical device manufacturing and services, research and testing, biotechnology, biopharmaceuticals, advanced diagnostics, and healthIT, amongst others; and are a key driver of Utah’s economy and life-saving treatments and cures for patients. BioHive is a chartered organization of BioUtah. Its mission is to brand, build and bring together Utah’s life sciences and healthcare innovation community. For more, visit https://bioutah.org/.
Media Contacts:
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
Lisa Barbadora, +1 (610) 420-3413, lbarbadora@barbadoraink.com
Curavit Earns HIPAA Seal of Compliance
Januayr 10, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
BOSTON – January 5, 2022— Curavit Clinical Research announced today that it has taken all necessary steps to prove its good faith effort to achieve compliance with the Health Insurance Portability and Accountability Act (HIPAA). Through the use of Compliancy Group’s proprietary HIPAA solution, The Guard™, Curavit can track its compliance program and has earned its Seal of Compliance™.
The Seal of Compliance is issued to organizations that have implemented an effective HIPAA compliance program using The Guard. HIPAA is made up of a set of regulatory standards governing the security, privacy, and integrity of sensitive healthcare data called protected health information (PHI). PHI is any individually identifiable healthcare-related information. If vendors who service healthcare clients come into contact with PHI in any way, those vendors must be HIPAA compliant.
Curavit has completed Compliancy Group’s Implementation Program, adhering to the necessary regulatory standards outlined in the HIPAA Privacy Rule, Security Rule, Breach Notification Rule, Omnibus Rule, and HITECH. Compliancy Group has verified Curavit’s good faith effort to achieve HIPAA compliance through The Guard.
“HIPAA compliance is imperative for clinical research, increasingly so as the clinical trial model becomes more decentralized,” said Joel Morse, co-founder and CEO of Curavit. “As a virtual contract research organization that designs clinical trials from digital first principles, we take patient privacy very seriously, and have built our always–audit-ready platform on validated technologies that support our HIPPA compliant processes.”
According to a statement by Compliancy Group, “Clients and patients are becoming more aware of HIPAA compliance requirements and how the regulation protects their personal information. Forward-thinking providers like Curavit choose the Seal of Compliance to differentiate their services.”
About Curavit
Curavit Clinical Research is a virtual contract research organization (VCRO) that designs and executes Decentralized Clinical Trials (DCTs) from digital first principles. Founded by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, minimizing the need for physical infrastructure and travel while increasing data quality and reducing patient burden. Curavit brings together the world’s leading researchers, enrolls previously underrepresented and underserved patient populations, and applies machine learning to health and social engagement information to recruit participants. For more information, visit www.curavitclinicalresearch.com.
Media Contact: Lisa Barbadora (610) 420-3413 lbarbadora@barbadoraink.com
Curavit Expands Leadership and Sales Teams to Drive Continued Growth of Decentralized Clinical Trials Across Life Sciences Industry
September 29, 2021

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
BOSTON— Sept.29, 2021 — Curavit Clinical Research, a virtual contract research organization (VCRO) that designs and executes decentralized clinical trials (DCTs), announced today the appointments of Jay Collier, as chief operating officer (COO), and Candice Del Rio, as director of clinical operations. The company also expanded its sales team with the hiring of industry veterans, Chris O’Shaughnessy, as vice president of business development, as well as Troy Hall and Bill Dreyer, as directors of business development. The expansion comes as DCTs continue their steady growth, punctuated by Curavit’s doubling its revenue since 2020.
Curavit continues to disrupt clinical research by enabling digitally native DCTs that expand trial access to previously underserved patients while improving patient participation, data quality, and research speed.
Jay Collier brings more than 20 years of operational experience serving global clients in life sciences and clinical research. In his role as COO, he will manage all aspects of service delivery for Curavit’s clients. Prior to joining Curavit, Collier served in various leadership positions, most recently senior vice president of U.S. operations at C3i Solutions, a global leader in healthcare technology services. C3i was also founded by Curavit’s co-founders, Joel Morse and Dave Hannaman, who sold the company to a Fortune Global 500 company in 2018. Before C3i, Collier served in various director-level roles at Nextel.
“Having worked with Joel and Dave for nearly 20 years at their previous company, I’m excited to join Curavit to help build another successful venture that will streamline the clinical trial process with advanced technology, and essentially improve global health and save lives,” said Collier. “This is a huge opportunity to make a meaningful difference in clinical research for years to come.”
Candice Del Rio, Curavit’s new director of clinical operations, has more than 12 years of clinical research experience in academic , clinical, and industry settings. Prior to joining Curavit, she worked at Massachusetts General Hospital as a clinical research nurse and an oncology/hematology nurse for over a decade. She will bring her in-depth experience in the areas of clinical trial development, patient recruitment and retention, and process improvement to manage projects and ensure customer success.
In addition, Curavit welcomes Chris O’Shaughnessy, as vice president of business development, who also comes from C3i Solutions; Bill Dreyer, as director of business development, previously manager of business development for EPL Archives, Inc.; and Troy Hall, as director of business development, who last served as a cardiovascular institutional specialist at Johnson & Johnson.
“It’s an exciting time at Curavit as we grow along with the rapid evolution and adoption of decentralized clinical research,” said Joel Morse, co-founder and CEO of Curavit. “We are taking it to the next level and our new team members will bring their collective expertise to help drive innovation and customer satisfaction, while delivering our scalable and purpose built clinical trial platform to our clients.”
In other news today, Curavit announces its membership into the Decentralized Trials and Research Alliance (DTRA). The DTRA includes 100 organizational members who represent the diverse ecosystem needed for the adoption of decentralized research methods, including sponsors, regulatory authorities, patient advocacy groups, contract resource organizations, technology companies, investigator sites, and other key stakeholders.
About Curavit
Curavit Clinical Research is a virtual contract research organization (VCRO) that designs and executes Decentralized Clinical Trials (DCTs). Founded by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, minimizing the need for physical infrastructure and travel while increasing data quality. Curavit brings together the world’s leading researchers, enrolls previously untapped and underserved patient populations, and applies machine learning to health and social engagement information to recruit participants. Current clients include Frequency Therapeutics, Beech Tree Laboratories, Brown University, and Boston Medical Center. For more information, visit www.curavitclinicalresearch.com.
Media Contacts:
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
Lisa Barbadora, +1 (610) 420-3413, lbarbadora@barbadoraink.com
First All-Virtual CRO, Curavit, Joins the Decentralized Trials & Research Alliance
September 29, 2021

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
BOSTON— Sept. 29, 2021 — Curavit Clinical Research, a virtual contract research organization (VCRO) that designs and executes decentralized clinical trials (DCTs), announced today that it has joined the Decentralized Trial & Research Alliance (DTRA) to further the advancement and adoption of decentralized clinicals.
Established in 2020, the DTRA enables collaboration of stakeholders to accelerate the adoption of patient-focused, decentralized clinical trials and research within life sciences and healthcare through education and research. It works to make research participation accessible to everyone, enabled by the consistent, widespread adoption of appropriate decentralized research methods.
“We are extremely gratified to welcome Curavit to the ‘Decentralized Trials & Research Alliance,’ said Amir Kalali, MD, founder of several collaborative life science communities, and co-Chair of DTRA. “By advancing decentralized research we can make the clinical trial process more patient-focused, increase trial efficiency and encourage use of technologies. We are excited by Curavit’s commitment to embracing decentralized trials and to changing the culture that has been the rate limiter to innovation.”
“This is an important opportunity for Curavit to collaborate with other DCT pioneers to further our mutual mission of making patient participation more accessible across all demographics,” said Joel Morse, co-founder and CEO of Curavit. “We look forward to sharing best practices, research methodologies, and technologies that will transform how research gets done.”
About Curavit
Curavit Clinical Research is a virtual contract research organization (VCRO) that designs and executes Decentralized Clinical Trials (DCTs). Founded by experts with decades of experience in technology and clinical research, Curavit leverages emerging technologies in digital health, cloud computing, and data science to recruit, engage, and monitor diverse patient populations without borders, minimizing the need for physical infrastructure and travel while increasing data quality. Curavit brings together the world’s leading researchers, enrolls previously untapped and underserved patient populations, and applies machine learning to health and social engagement information to recruit participants. Current clients include Frequency Therapeutics, Beech Tree Laboratories, Brown University, and Boston Medical Center. For more information, visit www.curavitclinicalresearch.com.
Media Contacts:
Jamie Dabao Brown, +1 (626) 488-0732, jamie@barbadoraink.com
Lisa Barbadora, +1 (610) 420-3413, lbarbadora@barbadoraink.com
Beech Tree Labs selects Curavit Clinical Research for fully virtual COVID-19 clinical trial
September 18, 2022

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
Curavit chosen for expertise in decentralized trial design and execution.
Beechtree Labs has chosen Curavit Clinical Research for a fully decentralized clinical trial to investigate a promising Covid-19 therapy. The FDA-authorized phase 2 clinical study will evaluate the effect of Beech Tree’s BTL-TML therapy on mean duration and severity of disease in 40 outpatients aged 60 years or older with underlying conditions. The study also assesses the safety of BTL-TML over 10 days of treatment and an additional four days of follow-up.
The trial is unique in that it is a fully decentralized clinical trial, made possible by applying virtual trial design protocols, digital telehealth technologies, electronic patient reported outcomes (ePRO), and full web and contact center patient support to eliminate the need for in-person office visits.
Thomas Hatch, Director of Business Development at Beech Tree said: “We chose Curavit because of their exclusive focus on designing and executing virtual trials. We needed a company with Curavit’s expertise in this important new discipline of clinical research in order to make this trial possible.” Joel Morse, CEO of Curavit added: “This is a unique opportunity to apply modern trial design and telehealth
technologies to allow patients to participate in this study without the potential risk of traveling to physical sites and to participate from the safety and comfort of their own homes.”
ABOUT CURAVIT
Curavit is a new type of clinical research company that designs and executes decentralized – also called “virtual” – clinical trials. Curavit brings together the world’s leading researchers, enrolls previously untapped and underserved patient populations, applies machine learning algorithms to health and social
engagement information, and leverages leading telehealth, patient data platform, and medical device technologies. Connect: https://www.linkedin.com/company/curavit/
Follow: https://twitter.com/CuravitClinical
ABOUT BEECHTREE LABS
Located in Providence, RI, Beech Tree Labs, Inc. (BTL) focuses on the discovery and early development of therapeutic agents that address a spectrum of unmet medical needs. The company has an extensive portfolio of patented formulations for products intended to treat such disorders as urinary incontinence, allergies, benign prostatic hypertrophy, anxiety, chronic obstructive pulmonary disease and herpesvirus infections. BTL has conducted over 15 FDA- authorized phase 2 trials and has out-licensed both technology and products.
LEARN MORE ABOUT THIS STUDY
The current FDA-approved Phase II pilot study is taking place in Draper, Utah at Intermountain Clinical Research. Additional sites will open in the future. To learn more about this study:
● You or your doctor may contact the study research staff ( deann@icrtrials.com ) or call
833-358-3784.
● Visit the study website: https://www.sickwithcoronavirus.com/
● You can also visit clinicaltrials.gov, the U.S. National Library of Medicine database of clinical studies conducted around the world. ClinicalTrials.gov identifier (NCT number): NCT04522830
MEDIA CONTACT
Dave Hanaman, Chief Commercial Officer, Curavit
info@curavitclinicalresearch.com
Curavit Clinical Research and eMoyo USA, LLC Partner to Deliver High-Quality Home-Based Audiometric Data for Virtual Clinical Trials
September 9, 2020

There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
New solution allows patients to participate in clinical trials from the comfort and safety of their own homes.
Curavit Clinical Research, a virtual research organization, and eMoyo USA, LLC, the USA representative of eMoyo, a global leader in healthcare technology, today
announced a partnership to pave the way for hearing research studies to continue
during the COVID-19 pandemic. Curavit’s virtual team of audiologists remotely monitor the hearing of research subjects in their homes using the eMoyo KUDUwave™ Pro boothless audiometer. This portable, high-frequency audiometer enables a booth-free operation and extended high frequency hearing test up to 16 kHz, making the KUDUwave™ Pro the ideal solution for virtual or hybrid clinical trials which require audiology end points.
“With KUDUwave™ boothless diagnostic audiometers we can now test patients in their homes without compromising on the quality of testing and without having to transport and maintain an audiometric booth. Given COVID-19, this provides a lower health risk for the study subjects, as the soundbooth could be a source of cross contamination.” says Grant Talbot, of eMoyo.
Prior to every planned audiology test date, a Curavit Study Team member sends a
pre-configured laptop and a KUDUwave headset to each study subject’s home. Working directly with the study subject, a Curavit audiologist initiates a telemedicine visit where they perform a thorough, high quality audiometric evaluation. The final data is securely transferred to the Curavit Study Team, where it is stored in a secure and validated system.
“With this unique technology, teamwork, and our proprietary protocols, a clinical trial subject performs a comprehensive hearing test in less than an hour, all from the comfort of their home,” said Dr. Pam Diamond, Otolaryngologist, co-founder and Chief Medical Officer of Curavit. “KUDUwave combines the audiometer, headset and required components into a single, portable, lightweight device weighing only half a pound and it is controlled remotely by our audiologists using a laptop and telemedicine software. This process may shorten the trial timeline, and minimizes the potential for trial disruption due to COVID-19.”
“We are honored to partner with eMoyo and to work together to bring these
best-in-class offerings to virtual and hybrid clinical trials. Though catalyzed by the
coronavirus pandemic, this solution makes participation in these types of trials far easier for many more patients, regardless of where they live, work and study; thus ensuring richer data and better research outcomes well into the future.” says Dave Hanaman, Chief Commercial Officer and co-founder of Curavit.
About Curavit Clinical Research
Curavit is a new type of clinical research company that designs and executes decentralized – also called “virtual” trials. Curavit brings together the world’s leading researchers, enrolls previously untapped and underserved patient populations, applies machine learning algorithms to health and social engagement information, and leverages leading telehealth, patient data platform, and medical device technologies.
https://curavitclinicalresearch.com/
About eMoyo
eMoyo is a team of passionate designers, engineers, clinicians and dreamers working to make the world a better place, by creating the technology that gives the world access to quality healthcare. This includes advocating for policy change, health implementation science and the development of technology that empowers healthcare providers to reach further and do more. Founded by Dr Dirk Koekemoer, eMoyo is an ISO13485 company renowned for producing high quality, innovative technology and services. https://emoyo.net/
MEDIA CONTACT
Dave Hanaman, Chief Commercial Officer, Curavit
info@curavitclinicalresearch.com
Curavit Clinical Research officially launches with a focus on virtual trials
February 18, 2020
There’s more than one way to architect a decentralized clinical trial (DCT). While this flexible model has many benefits, it can be overwhelming to bring together all the right elements to operationalize a trial that’s predominantly digital. Every trial is unique, so it is not realistic to templatize (impose a standard implementation template on) a DCT. But four common, fundamental components combine to facilitate a seamless, patient-centric DCT.
“It’s like a trial in a box, but each box is a little bit different,” said Steve Rosenberg, CEO of a cloud-based platform company that powers decentralized clinical trials. Even with a DCT’s inherent optionality, foundational components can ease implementation and improve execution.
Industry veterans Joel Morse and Dave Hanaman announce the formation of a company to lead into the future of clinical trials.
Curavit was founded to help realize the potential of decentralized trials. Mssrs. Morse and Hanaman come to Curavit with over twenty five years of experience, founding, building, and running successful technology-enabled healthcare companies. https://curavitclinicalresearch.com/about
● The $70 billion global clinical trials market continues to grow , while the success rate of trials continues to decline, often due to lack of enrollment and participation by patients and doctors.
● New technologies and new approaches offer an opportunity to both increase success rates and decrease the costs of traditional clinical trials.
● Virtual clinical trials take advantage of these trends and opportunities.
● Just a small percentage of trials today, virtual trials are projected to increase geometrically due to their advantages.
“Curavit is the result of our desire to solve growing challenges to the important work of drug discovery.” said Joel Morse , Chief Executive Officer and Co-Founder of Curavit. “By combining experience, technology, and solid execution, we will bring cutting-edge research to previously untapped and underserved patient populations.” Chief Commercial Officer and Co-Founder Dave Hanaman added:
“We are fortunate to have worked with some of the most respected companies and visionary people in the life sciences industry, and are honored by the support we are receiving from them for this effort.”
ABOUT CURAVIT
Curavit Clinical Research takes a clean sheet approach to clinical trial design and execution. Optimized on a new “virtual” – or decentralized – model, the company supports patients’ participation from wherever they live, across the country, and around the globe. Curavit teams with distinguished principal investigators in specific therapeutic classes, works from archetypal investigational sites in major research hubs, leverages best-in-class industry standard patient data platforms and mobile health devices to collect, manage and protect patient data. By applying advanced data analytic algorithms to patient information and real world evidence, Curavit partners with healthcare entities to identify, qualify, and enroll patients in approved clinical trials. Curavit plans to open its first site in Boston this summer.
Connect: https://www.linkedin.com/company/curavit/
Follow: https://twitter.com/CuravitClinical
MEDIA CONTACT
Dave Hanaman, Chief Commercial Officer
info@curavitclinicalresearch.com
Contact Curavit
Let’s Talk